Do These Donated Embryos Make the Grade?
Embryo Grading Made Easy For Embryo Donors and Embryo Recipients
Part 1 of a 3 part mini-series by Corey Burke, B.S., C.L.S. & Laboratory Supervisor and Reproductive Endocrinologist Craig R. Sweet, M.D.
Embryo grading is an important factor for both donors and recipients. Potential embryo donors want to know if we will accept their embryos for donation since part of our decision is based on the grade of their embryos. Likewise, potential embryo recipients want to know how likely the donated embryos are to survive thawing and if they are of good enough quality to build their family. Part of our estimation of success depends on the grade of the embryos.
We wish this process could be easier since there is no standardized system used in all embryology laboratories to grade embryos. Furthermore, the grading of embryos is somewhat subjective so one embryologist may grade an embryo
somewhat differently than a colleague.
Embryo grading is an imperfect process; poorly graded embryos may occasionally result in ongoing pregnancies and beautiful looking embryos may not implant and grow. Poorer graded embryos will not necessarily result in an abnormal child; they simply seem to implant and grow less frequently.
So, the appearance and grading of an embryo is an imperfect estimate of the quality of the embryo as well as the embryo’s true potential. It is, however, the best way we have to visually estimate the implantation and live birth rate of a given embryo. We will now examine one of the more common methods used to grade embryos.
When are embryos graded and cryopreserved?
Embryos are usually graded and frozen at three specific stages with “Day 0” being the day of retrieval and fertilization:
| Age of Embryos | Day 1 | Day 3 | Day 5-6 |
| Common terminology | 2PN (pronuclear stage)
2 cell stage |
Embryos are 6-10 cells | Morula &
Blastocysts |
| Grading importance | Grading not available | Grading relatively important | Grading very important |
| How often these are sent to EDI? | Rarely sent | 40% of EDI embryos | 60% of embryos |
Embryos cryopreserved immediately after fertilization are confirmed early on Day 1 (the 2PN (pronuclear stage), but aren’t advanced enough to be consistently graded. Freezing embryos on Day 1 is quite infrequent unless we are certain there will not be an embryo transfer. Accordingly, these embryos are rarely sent to EDI for embryo donation.
Grading Day 3 Embryos
Day 3 embryos are graded on cell number, the amount of cellular fragmentation and the symmetry of the embryo.
Cell Number
Most Day 3 embryos will be comprised of 6-10 cells called blastomeres. Embryos with too few blastomeres may not be healthy, so we prefer at least 7-8 at this stage. Embryos with fewer cells may not be healthy growing very slowly or may have stopped growing entirely commonly called “cell block”.
Fragmentation
Fragments may be found in many of the embryos, which are “bits” of cells that break off from a blastomere. We prefer as little fragmentation as possible. Fragmentation is estimated as the percentage of fragmentation volume compared to the total embryo volume and is converted to a letter grade in the following way:
- 0 % = A
- 1-10% = B
- 11-25% = C
- >25% = D
A large amount of fragmentation may be caused by death of one or more of the blastomeres. The higher the fragmentation, the lower the quality of the embryo & letter grade and the less likely that the embryos will survive thawing. Embryos with high fragmentation rates implant less frequently when transferred fresh or when thawed.
Symmetry
Symmetry of the embryo refers to the shape of the individual blastomeres and the overall shape of the embryo. The blastomeres should all be very similar in size and generally round in shape. The scale used to grade symmetry is
- Perfect = A
- Moderately asymmetric = B
- Severely asymmetric = C
Severe blastomere asymmetry (i.e., large and small blastomeres in the same embryo) reflect nuclear/chromosomal and cytoplasmic problems suggesting the embryo is less healthy than desired. There is supporting evidence that blastomere symmetry is important and reflects overall health of the embryo. Interestingly, the overall symmetry of the embryo (round vs. oval) is of uncertain importance with some very “funny looking” embryos resulting in beautiful and healthy children.
Putting it All Together for Day 3 Embryos
For Day 3 embryos, the order of grading is the “number of cells (#c),” “fragmentation grade” and “symmetry grade”. For example:
- 7cAA = 7 cells with no significant fragmentation and perfect symmetry
- 8cBA = 8 cells with 1-10% fragmentation and perfect symmetry
- 6cBB = 6 cells with 1-10% fragmentation and moderate asymmetry.
Grading Day 5 Embryos
More advanced embryos are graded and potentially frozen on Day 5 or Day 6. These are generally described as morula or blastocysts.
Day 5 Morula Embryos
Morula embryos are difficult to grade as the cells combine, forming essentially a ball of cells that can’t really be categorized in any way other than descriptive terms:
- Morula (early)
- Compacting morula (more advanced)
While some facilities only occasionally cryopreserve Day 5 morula embryos, it is thought that the survival and implantation rates of these embryos may be slightly reduced but they are still quite reasonable, suggesting that they should not be discarded. Day 6 morulas are probably delayed in growth or may have stopped growing, may not be viable and are infrequently cryopreserved.
In order to balance the possible reduced implantation rates, it is common that more morula embryos are thawed and transferred in order to achieve success.
Day 5 Blastocyst Embryos
Day 5 blastocyst embryos are the most advanced embryos we see in IVF. These embryos are formed within 24 hour of actual implantation. Trying to grow embryos beyond this point is
technically difficult, as the embryos usually don’t survive. In addition, the window of time for implantation seemingly closes beyond Day 5 or early day 6. For example, transfer on Day 7 will rarely result in implantation. So, it simply makes more sense to transfer and/or freeze blastocysts rather than trying to grow them any further.
Along with descriptive measures, more objective grading is attempted through evaluation of the cellular expansion, the inner cell mass (which eventually becomes the fetus) and the quality of the outer cell mass called the trophectoderm (which eventually forms the membranes and placenta).
Expansion
As the embryo advances in growth, a cavity called the blastocoel fills with fluid. As the cells continue to divide and the fluid collects, the embryo expands and eventually escapes its outer covering called the zona pellucida. The blastomeres continue to group together wherein the individual cell cannot be counted. As the Day 5 embryo expands, differentiates and escapes the outer zona pellucida, the grade increases numerically from 1-5.
| Grade | Description | Physiology |
| 1 | Early Blastocyst | Starting to form a fluid-filled space in the middle (Blastocoel). Grading the embryo is difficult here. |
| 2 | Full Blastocyst | Blastocoel forms and inner cell mass is now distinguishable. Grading can be done from this point forward. |
| 3 | Expanded Blastocyst | Blastocyst is starting to expand in size thinning the outer covering, the zona pellucida |
| 4 | Hatching Blastocyst | Blastocyst is starting to hatch out of the zona pellucida. |
| 5 | Hatched Blastocyst | Blastocyst is fully hatched and now ready for implantation into the uterine wall. |
Inner Cell Mass (ICM)
As the blastomeres compact to form the inner cell mass (ICM), this early fetal tissue is graded on a A-D scale:
| ICM Grade | Description |
| A | ICM with total compaction |
| B | ICM still compacting |
| C | Reduced ICM |
| D | Poor with dying cells |
Trophectoderm (TE)
The outer cells of the trophectoderm (TE) also reflect the overall health of the embryo and are graded in an A-D scale.
| TE Grade | Description |
| A | Numerous cells forming cohesive layer |
| B | Few but healthy large cells forming a loose epithelium |
| C | Few cells present often with asymmetric distribution |
| D | Poor with degenerating/dying cells |
Putting it All Together for Day 5 Embryos
For Day 5 embryos, the order of grading is “expansion,” “inner cell mass” and “trophectoderm.” For example:
- 1 = Early blastocyst is unable to be easily graded with respect to ICM or TE as these haven’t separated well enough yet.
- 2BB = Blastocyst with partial ICM compaction with loose, large trophectoderm cells
- 3AB = Expanding blastocyst with total compaction of ICM and with loose, large trophectoderm cells
- 4AA = Hatching blastocyst with excellent ICM & trophectoderm cell layers
- 5AA = Fully hatched blastocyst with excellent ICM & trophectoderm cell layers
Day 5 embryos that are graded 4AA and 5AA are some of our favorite embryos.
Summary Comments
Embryology laboratories strive to grow the healthiest embryos they can. Over time, they have adapted different grading techniques so the laboratories can communicate the quality of the embryos to physicians, patients and each other. Not all beautiful embryos will implant or produce a healthy child but they seem to do so more often than others. Not all poorly developing embryos will fail to implant and produce a healthy child but most do not result in live offspring.
At EDI, we try to only accept embryos that are likely to implant so embryos with less than a B rating for any category are infrequently accepted. This is done to assure our recipients that all of the donated embryos we offer are of the highest quality and provided the greatest chance for a successful pregnancy.
This is only one piece of the puzzle as many other factors influence the likelihood for success. Dr. Sweet will cover this topic in the separate blog within the next couple of months.
Also stay tuned to the upcoming blogs regarding how embryos are frozen and thawed and what techniques seem to work the best.
While embryo grading is not a perfect system, we use it to try to predict the overall quality of the embryos and their potential to survive thaw, grow and build a recipient’s family.
Corey Burke. B.S., C.L.S.
Laboratory Supervisor
CBurke@EmbryoDonation.com
Craig R. Sweet, M.D.
Reproductive Endocrinologist
Info@EmbryoDonation.com
References
Racowsky C, Vernon M, Mayer J, Ball GD, Behr B, Pomeroy KO, Wininger D, Gibbons W, Conaghan J, Stern JE. Standardization of grading embryo morphology. Fertil Steril. 2010 Aug;94(3):1152-3.
3 Responses to “Do These Donated Embryos Make the Grade?”
New Mini-Series on How Embryos are Processed
 Beginning next week, we’ll be publishing a mini-series on how embryos are processed in the laboratory. Written by Corey Burke, B.S., C.L.S. & Laboratory Supervisor and Reproductive Endocrinologist Craig R. Sweet, M.D., the three-part series will cover how embryos are initially graded, frozen and finally thawed. The information is designed for patients and written in an easy to understand style.
Beginning next week, we’ll be publishing a mini-series on how embryos are processed in the laboratory. Written by Corey Burke, B.S., C.L.S. & Laboratory Supervisor and Reproductive Endocrinologist Craig R. Sweet, M.D., the three-part series will cover how embryos are initially graded, frozen and finally thawed. The information is designed for patients and written in an easy to understand style.
We hope this will be an informative series, answering many common questions alike. If you have additional questions, please feel free to post them as comments here, or after the specific blog post.
Thank you for reading and stay tuned for detailed embryo grading, freezing and thawing information starting with the first series post on Tuesday, January 10th.
–Embryo Donation International
How Does Embryo Donation International Rank Embryo Recipients?
Unfortunately, there are far more potential embryo recipients than donated embryos. While in this country alone, hundred of thousands of embryos are stored in liquid nitrogen, (Hoffman DI, et. al, 2003), less than ten percent and frequently less than five percent are donated to patients in need (Klock SC, et al., 2003). As a result, we often have a waiting list of recipients asking for donated embryos.
First, EDI doesn’t discriminate with respect to race, religion, ancestry, sexual preference or  marital status. We also try to be fair to existing EDI patients and to those who have yet to become established patients. We basically are looking for potential embryo recipients who have few other reproductive options available. If one views donated embryos as an essentially rationed commodity, we want to make certain that patients in greatest need are ranked the highest. We try to do this in an ethical and fair fashion but ranking them can be a challenge.
marital status. We also try to be fair to existing EDI patients and to those who have yet to become established patients. We basically are looking for potential embryo recipients who have few other reproductive options available. If one views donated embryos as an essentially rationed commodity, we want to make certain that patients in greatest need are ranked the highest. We try to do this in an ethical and fair fashion but ranking them can be a challenge.
While not absolute, below is a general ranking from high priority to lower priority in our general waiting lists:
- The intended parents have no delivered children and limited financial means with few options available.
- Their only child died and no other siblings exist.
- One of the partners raised a child with a different partner.
- Both of the partners raised children with different partners.
- Both partners raised one adopted child together.
- Both partners raised one (genetic) child together.
- Both partners raised children with other partners and one (genetic) child together.
- Both partners raised multiple (genetic) children together.
We define a “genetic child” as a child whose genes came from the parents themselves without the use of donated material and also not an adopted child.
Here are some of the questions we also commonly ask in trying to decide where the patients should rank on our waiting lists:
- How long have they been on the waiting list?
- Are they established patients with EDI or have never been seen before?
- Are there other less expensive and viable options such as donor sperm?
- What have the patients gone through during their infertility journey?
- Is adoption of a live child a possibility?
- Are there financial constraints that makes embryo donation far more feasible over other more expensive options?
Also, we actually have multiple lists broken down by the following major categories:
- Type of embryo donation: Anonymous, Approved and Open Embryo Donation
- Marital status/sexual orientation: Single woman, single man (very rare), heterosexual couple (married/unmarried), lesbian couple and gay couple (married/unmarried).
 As you can see, the process of ranking can get a bit complicated. Our highest priority is healthy embryo recipients who have never had children of their own and have very few fertility options with limited financial means. For example, this group may include cancer survivors who have been left infertile due to the disease or treatment. In many states, cancer survivors find adoption of a child extraordinarily difficult, so embryo donation may be their only option for building a family. We also tend to rank patients higher who have undergone extensive unsuccessful IVF treatments and egg donation is their only remaining option, but due to financial constraints, are unable to afford the procedure.
As you can see, the process of ranking can get a bit complicated. Our highest priority is healthy embryo recipients who have never had children of their own and have very few fertility options with limited financial means. For example, this group may include cancer survivors who have been left infertile due to the disease or treatment. In many states, cancer survivors find adoption of a child extraordinarily difficult, so embryo donation may be their only option for building a family. We also tend to rank patients higher who have undergone extensive unsuccessful IVF treatments and egg donation is their only remaining option, but due to financial constraints, are unable to afford the procedure.
While we do not exclude patients who have raised children, some requests come from parents with numerous children in their current family. We are actually not looking for potential embryo recipients who are trying to “save” donated embryos. We wish we had enough embryos for everyone, but until we have more embryos than applicants, we will continue to prioritize patients who have never raised children higher than those who have previously experienced the joys of parenthood. We will not exclude such patients, they will be ranked far lower than others on the priority scale.
While some patients who approach EDI have no children, they may have several other fertility options. For example, a young couple that is infertile due to severe male factor infertility, may best be served with sperm donation. Donor sperm generally is less expensive and faster than embryo donation and they can have more than one child using the same donor. We would prefer to save the donated embryos for patients with few available options.
We hope that our readers will understand our basic goals. For any rationed commodity, we want to save it for those in greatest need. If one pictures the embryos as rare, precious and hard to come by, one can imagine why a fair ranking system must be developed.
Ranking systems are never perfect and often seem unfair to those who receive lower rankings. It is difficult to explain a lower ranking to a patient who is desperately seeking to build or expand their family, however, once separated from the emotional aspect, it is usually agreed that a ranking system is needed to fairly as many patients that we can who are seeking donated embryos.
In summary, we feel that a ranking system is necessary to achieve our goal of matching donated embryos to patients in need in an ethical and fair fashion. In a perfect world, infertility wouldn’t even exist and there would be enough donated embryos to meet the demands of those asking for donated embryos. In today’s realistic world, however, the precious gift of donated embryos is simply not given often enough to meet the demands of those seeking donated embryos. Perhaps someday ,though education and research, the number of patients offering their embryos for donation will increase to such a level that we may be able to eliminate or at least trim back segments of our ranking system. Until that day comes, we will have to do our best to assist in matching patients in need to donated embryos in the most ethical and fair fashion we can.
Shelley Osking, L.P.N.
Embryo Donation Coordinator
Shelley@EmbryoDonation.com
Corey Burke, B.S., C.L.S.
Laboratory Supervisor
CBurke@EmbryoDonation.com
Craig R. Sweet, M.D.
Reproductive Endocrinologist
Founder, Medical and Practice Director
Info@EmbryoDonation.com
Hoffman DI, et al. Cryopreserved embryos in the United States and their availability for research. Fertil Steril 2003;79:1063-9.
Klock SC, et al. The disposition of unused frozen embryos [letter]. N Engl J Med 2001;345(1):69-70.
4 Responses to “How Does Embryo Donation International Rank Embryo Recipients?”
-
Wow, this is a really interesting article, offering people insight into the world of embryo donation. Choosing which parents receive donated embryos is a heavy burden, but it sounds to me like your team has put a lot of thought and consideration into this ranking system.
Does EDI ever allow the genetic parents to choose the intended parents?
Sara R. Cohen
http://www.fertilitylawcanada.com
twitter @fertilitylaw
facebook http://www.facebook.com/FertilityLawCanada -
As a single woman, finding a donated embryo can be much more difficult than for a two parent family and I wonder if a single parent plays any role in the ranking?
Georgia Law: The First Salvo Towards Embryo Personhood
A Guest Post by: Harold Eskin, Esq.
New laws are beginning to appear on the books of many states that support “embryo adoption.” “Embryo Adoption” is placed in quotation marks because that phrase alone has unique connotations that I discuss briefly below. The term embryo “donation” is also a commonly used expression describing giving one patient’s/couple’s cryopreserved (frozen) embryo(s) to another patient/couple trying to expand their family, but who otherwise have been unsuccessful through natural and/or advanced reproductive techniques.
 Georgia was the first state to pass an embryo adoption bill (2009) that provided an opportunity for intended parents to go through an adoption procedure to obtain the right to gestate a thawed frozen embryo. Other states, such as Florida, have embryo donation statutes on its books, which allow a couple to receive a donation from another (open or anonymous) of a frozen embryo. While the end results may appear to be the same, the road getting there and implications of using the different phrases are vastly different.
Georgia was the first state to pass an embryo adoption bill (2009) that provided an opportunity for intended parents to go through an adoption procedure to obtain the right to gestate a thawed frozen embryo. Other states, such as Florida, have embryo donation statutes on its books, which allow a couple to receive a donation from another (open or anonymous) of a frozen embryo. While the end results may appear to be the same, the road getting there and implications of using the different phrases are vastly different.
The Georgia law, which was championed by Right to Life groups, treated a frozen embryo in much the same way as it would a child already born. The new law and procedures mimic that of other adoption provisions and gives the frozen embryo many of the same rights and considerations of a born child, including using a “best interest of the child” standard in the adoption analysis. This philosophy is consistent with the concept that a child’s rights (as compared to the mother’s) begins at conception rather than birth and has implications in the abortion-right to choose/right to life arguments ongoing disagreements and potential laws expressing same.
Florida and many other states have historically treated frozen embryos as the property of the parents, who have the right to donate or dispose of the frozen embryos as they saw fit. The recipients received the frozen embryos as property under the respective laws of their state and could use or dispose of the frozen embryos as they saw fit. This process allowed for freer access to unused frozen embryos and discouraged the abandonment/discarding of them.
The agenda of the Georgia law was not necessarily meant to “protect” the frozen embryos but was designed to advance a political agenda of creating additional barriers to a women’s right to choose (i.e. restrict abortion) and to further control the reproductive rights of patients by discouraging the use of advanced reproductive techniques, such as in vitro fertilization as well as the cryopreservation and storage of excess embryos.
Up to now, there have been few attempts to export the Georgia concept in other states. This is perhaps due to the country’s economic challenges, but this possible trend needs to be closely monitored. The implications of providing “personhood” to embryos are far and wide and the Georgia statute is one of the first successful salvos to be launched with others most certainly to follow. Mississippi is currently targeted for a constitutional amendment to give embryos personhood and many other states are next in line for challenges that may significantly impair the health and reproductive care of women.
Harold Eskin, Esq.
www.LegalSurrogacy.com
HalEskin@LegalSurrogacy.com
1420 SW 47th Street
Cape Coral, FL 33904
239-549-5551
References:
Georgia Statute:
http://statutes.laws.com/georgia/title-19/chapter-8/article-2/19-8-41Florida Statute:
http://www.leg.state.fl.us/Statutes/index.cfm?App_mode=Display_Statute&Search_String=&URL=0700-0799/0742/Sections/0742.14.html
2 Responses to “Georgia Law: The First Salvo Towards Embryo Personhood”
-
Go Georgia!
With scientific advancement and rights also come responsibility. Folks need to think carefully about what they’re doing when initiating new lives. If conception isn’t the beginning of life, what is? And who gets to decide? Is the decision then one of ethics, or convenience? There are a lot of little embryos out there, suspended in frozen time. Sadly not as many as you think are available for adoption because their owners aren’t comfortable with having their DNA out there with another family.
Hope & Will Have a Baby – Book review by Craig R. Sweet, M.D.
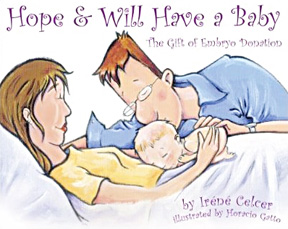 This book is one of a collection of third party conception children’s books written by the same author and illustrator and published by Graphite Press, copyright of 2006. It is one of the only books I have seen for children conceived though embryo donation.
This book is one of a collection of third party conception children’s books written by the same author and illustrator and published by Graphite Press, copyright of 2006. It is one of the only books I have seen for children conceived though embryo donation.
Ms. Celcer is a mental health professional that feels it is important to be up front in telling the children of embryo donation about their origin. In her forward, she cites the past secrets in adoption causing harm. She goes on suggesting that-
- • Children somehow sense the secrets
- • The failure to divulge may create shame in the parents of donated embryo offspring
- • Failure to tell a child results in a loss of pride of their beginnings
This book is to be used to tell the children about their loving conception while trying to manage the complex emotions of the parents.
Through the eyes of Hope and Will, a young married couple in love, the book explains what a “special place” the uterus is and how  embryos are created. Hope and Will experience infertility, depression and probably some grumpiness (can you imagine?). They seek help through Dr. Quest, who gives Hope tablets, pills and shots, but to no avail. Embryo donation is discussed, explaining anonymous and open options in simple and easy to understand terms.
embryos are created. Hope and Will experience infertility, depression and probably some grumpiness (can you imagine?). They seek help through Dr. Quest, who gives Hope tablets, pills and shots, but to no avail. Embryo donation is discussed, explaining anonymous and open options in simple and easy to understand terms.
Hope and Will conceive though embryo donation. The author emphasizes love, pride and excitement when the delivery finally takes place. Hope and Will are clearly grateful to their donor couple whom they have never met. Enough information is provided about the donors to help the child understand his origin.
While perhaps a little complex for a young child of four or five, the book might work quite well for a slightly older child. The pictures are wonderful and the emphasis on love and the desire to have a child by whatever means necessary is well done. I have always suggested that if parents tell the child, they should highlight their tremendous desire to have and love that child, as well as how hard they worked to bring such a wonderful child into their home.
Disclosure in embryo donation is a periodic theme of a number of my blogs. Adoption is clearly different than embryo donation. Adoption tends to be well accepted by most of the world’s religions. If embryo recipients tell friends, family and their donor-conceived offspring, there may be significant repercussions. Will the recipients and offspring be criticized, ostracized or, even, excommunicated by these same people or by their own religion?
Unfortunately at this time, I simply don’t believe we have enough data to make a clear recommendation to embryo recipients although there is wonderful ongoing research that will hopefully help to answer this question. For now, extrapolating what we have learned from adoption may simply not be appropriate for embryo donation, although passions on both sides of this issue  abound. The long-term consequences of secrecy vs. total openness to friends, family and the child of embryo donation are essentially unknown and I feel this decision needs to be made carefully with consultation with skilled mental health professionals (and Ms. Celcer is one of them), reproductive endocrinologists and perhaps, most importantly, recipients that have already traveled this journey.
abound. The long-term consequences of secrecy vs. total openness to friends, family and the child of embryo donation are essentially unknown and I feel this decision needs to be made carefully with consultation with skilled mental health professionals (and Ms. Celcer is one of them), reproductive endocrinologists and perhaps, most importantly, recipients that have already traveled this journey.
Selling for about $20 at Barnes & Noble, the purchaser should know this is a paperback and only 28 pages. The reader is clearly paying for the content and not story length or volume.
I highly recommend this book for those parents who decide to tell their child they were conceived through embryo donation, although the story line may need to be changed for single women and gay and lesbian couples. For the lucky parent(s) of embryo donation, this is a fairly good place to start if disclosure is the path they choose to follow.
Craig R. Sweet, M.D.
Founder, Medical & Practice Director
Embryo Donation International
2 Responses to “Hope & Will Have a Baby – Book review by Craig R. Sweet, M.D.”
-
As a single woman, finding a donated embryo can be much more difficult than for a two parent family and I wonder if a single parent plays any role in the ranking?
Disclosure Issues in Embryo Donation: Summary Comments
Brief Introduction
Embryo donors and recipients are faced with a number of life-changing decisions as they contemplate disclosure. This is the final segment of a five-part series summarizing the complex decisions surrounding the disclosure of the genetic origins of embryo donor-conceived individuals to family, friends and the offspring themselves.
What are some of the questions that embryo donors and recipients must explore before deciding to disclose or not?
Embryo donors must decide if they want a relationship with the donor-conceived individual being raised by another family. Are the donors willing to disclose their donation of embryos, which may have taken place years ago, to friends and family, including their existing children? At what age would they want the donor-conceived individual to contact them?
Recipients need to ask related questions about whether they should tell their embryo donor-conceived children about their origins. If they want to do so, when should they tell and what information should they share? Are the recipients comfortable letting their family members and friends know of their infertility history? Will the recipients and offspring be criticized, ostracized or, even, excommunicated by these same people or by their religion? Are they comfortable with their child contacting and potentially having a relationship with the embryo donors and their blood siblings?
Can an understanding of adoption disclosure be used in the world of embryo donation?
It is understandable, but potentially misguided, that some professionals believe embryo donation is identical to the adoption of a live child. I have written about this topic before. While the American Society for Reproductive Medicine (ASRM) states that the term “embryo adoption” should not be used, some facilities do so openly.
However, regardless of the legal differences, there also are a number of very practical differences:
- Because the embryo recipient carries and delivers the child, her pregnancy may look natural, making disclosure by the recipients optional. Adoption is much more difficult to hide.
- Disclosure of the embryo donation process may not be well accepted by friends, family and some religions. While not universally accepted, adoption may be better tolerated.
- As with sperm donation, single women and lesbian couples who conceive with donated embryos are more likely to disclose because the fatherhood issue inevitably arises. Heterosexual couples, however, are the least likely to disclose.
How often is disclosure currently revealed?
 There is a growing body of data that suggests only a minority of the embryo donor-conceived children are told of their origins. In an English study of 17 embryo donation families with donor offspring between five and nine years old, only 18% of the recipient parents had told their children (MacCallum F. et al. 2008). An additional 24% planned on telling, 12% were undecided and 47% stated they would not tell. The reality is that many of those who planned on telling or were undecided may eventually decide against disclosure as the child ages and enters the more difficult years of adolescence. This seemed to be different than other donor procedures where 46% of donor sperm insemination parents and 56% of egg donation parents planned to disclose (Golombok S, et al. 2004).
There is a growing body of data that suggests only a minority of the embryo donor-conceived children are told of their origins. In an English study of 17 embryo donation families with donor offspring between five and nine years old, only 18% of the recipient parents had told their children (MacCallum F. et al. 2008). An additional 24% planned on telling, 12% were undecided and 47% stated they would not tell. The reality is that many of those who planned on telling or were undecided may eventually decide against disclosure as the child ages and enters the more difficult years of adolescence. This seemed to be different than other donor procedures where 46% of donor sperm insemination parents and 56% of egg donation parents planned to disclose (Golombok S, et al. 2004).
Why has anonymity been the norm in embryo donation?
The concept of anonymity in egg/sperm/embryo donation has its roots in the physician/patient relationship to meet a series of needs (Daniels K. 1997). To assume that it should be discontinued for everyone doesn’t take into account the ethical, social and religious circumstances of different patients.
Since the medical profession assumes parents are able to make, without question, thousands of different choices for their children, assuming they are incapable of making a decision, such as disclosure which affects both the child and parents, is simplistic and rather paternalistic.
Why not disclose?
Let’s face it; there might indeed be a lack of societal approval of offspring who originated from donor material. Many people are judgmental regarding embryo donation, especially in cultures and religions that emphasize genetic inheritance. Recipients have legitimate reasons to fear the potential damage to themselves and their children from other people’s negative reactions, social stigma and resulting isolation (Shehab D, et al. 2008).
Some of the reasons recipients do not want to disclose include protecting their children  and family relationships from rejection, not feeling a need to disclose or uncertainty about how to approach the matter (MacCallum F, et al. 2007, Jadva V, et al. 2009 & Mahlstedt PP, et al. 2010). Disclosing also will broadcast their infertility issues, which they may have kept quite private in the past (Klock SC. 1997). Another common reason given for not disclosing is fear that they as non-genetic parents will be rejected. Actually, there is no data to support or deny this last very human concern.
and family relationships from rejection, not feeling a need to disclose or uncertainty about how to approach the matter (MacCallum F, et al. 2007, Jadva V, et al. 2009 & Mahlstedt PP, et al. 2010). Disclosing also will broadcast their infertility issues, which they may have kept quite private in the past (Klock SC. 1997). Another common reason given for not disclosing is fear that they as non-genetic parents will be rejected. Actually, there is no data to support or deny this last very human concern.
Unlike adoption, it is doubtful that the offspring of embryo donation will have to resolve the “history of rejection” unlike adopted children who were separated from their birth parents (Widdows H, et al. 2002). Families created through embryo donation are a product of a loving gift and not formed from perceived rejection. Therefore, some of the motivation to disclose in adoption simply does not exist in embryo donation.
Why should parents disclose?
The most common reason for embryo recipients to disclose is a fear that the child will accidently discover the facts at a later date (MacCallum F, et al. 2007). One study of adult offspring of sperm donation found that about 1/3rd of the individuals learned of their donor origins after an argument, from another person or they just figured it out themselves (Mahlstedt PP, et al. 2010). In a recent study, about 10% (47/458) of the sperm donor offspring who were searching for their donors and half-siblings found out by accident (Beeson DR, et al. 2011). They were apparently told by siblings, family or friends; discovered paperwork or inheritable medical issues that their recipient parents did not have; inadvertently overheard their parents talk about it; or it was revealed as a consequence of divorce. Recipients who tell family and friends but not the child are asking for future problems. When examining these two studies, it is clear there is a reasonable risk that the offspring will discover their origins, even under the best of circumstances. It also is important to realize that sperm, egg and embryo donation procedures are different when analyzing the study results.
There are some embryo donation recipients who feel it is simply best to not have secrets in the home. Others believe the embryo donor-conceived children have a moral right to know their origins. Some feel it is important that the children understand and connect to their genetic inheritance beyond the family who raised them.
What should be disclosed?
There are three decision levels in disclosure: 1) To decide to disclose, 2) To decide what age to disclose, and 3) To decide what information is to be provided. One can simply tell the child he or she was embryo donor-conceived but the child is certain to have more questions. At the very least, I believe providing the donors’ photographs (when they are available) as well as their medical, surgical, psychiatric, family and social histories are needed. However, providing actual identifying information needs to be handled carefully and thoughtfully.
When should disclosure take place?
Disclosure early in the child’s development, certainly before age ten, would seem to be ideal. Some mental health professionals (MHP’s) feel it should be discussed as early as possible. If disclosure occurs in adolescence or later, young adults may feel mistrust, alienation, identity confusion, frustration and even hostility towards their family (Ethics Committee, 2004 & Mahlstedt PP, et al. 2010). About 46% of donor sperm offspring who were told at the age of 18 or older stated they were confused. It is probably best to tell the child before the age of 10 than wait until later where there is a doubling of the number of children who were unsettled with the information.
Why do embryo donor-conceived individuals want to know their genetic origins?
Many embryo donor-conceived individuals may be curious about their donors’ physical characteristics and original motivation to donate, as well as possess a desire to know their genetic identity and, perhaps, provide an ancestral history for their own children. (Ravitsky V, et al. 2010 & Mahlstedt PP, et. al. 2010).
For many, the search for their donors may go well beyond just seeking simple information. In two recent studies of offspring searching for their donor sperm fathers, 80-88% were intensely curious about their donor and wanted to contact him. Up to one-third desired an actual relationship with the sperm donor (Beeson DR. 2011 & Mahlstedt PP, et al. 2010). It should be understood, however, that studies such as these might not represent a balanced patient sample. Only offspring searching for information contributed to those studies. There wasn’t a practical way to capture the opinions of those offspring who were not part of the Internet support groups, who may indeed represent a very silent majority.
Do embryo donor-conceived offspring have the right to know their origins?
Many donor-conceived individuals feel they have a right to know their genetic origins (Shehab D, et al. 2008). Embryo donors and recipients, who may prefer an anonymous process, have rights that compete with those of the donor-conceived individuals. Embryo donors and recipients have legal rights that are in direct contrast to the offspring’s moral view that family secrets shouldn’t be kept. There is no easy way to reconcile these contrasting legal rights and moral perspectives. Most agree, at the risk of offending those who feel differently, that in a society ruled by law, a legal right ultimately trumps a perceived moral right. Thus, the legal rights of donors and recipients continue to prevail in this country.
Should disclosure be mandated?
There is a stronger preference to discard or abandon the embryos than there is to donate them. Placing any impediments on embryo donation, such as mandating disclosure, may not only reduce the number of embryos donated but will almost certainly result in a greater number of embryos discarded or abandoned. I cannot imagine the well-meaning individuals who are asking for mandated disclosure would want the loss of embryos and potential families to be an almost certain unintended consequence.
Parents who used donor material feel the decision to disclose is private, highly personal and should be left to the discretion of the individual families and not regulated in any way (Shehab D, et al. 2008). A dual-track of disclosure/nondisclosure system will most meet the needs of everyone (De Jonge C, et al. 2006). We need to educate, guide and support, but not force these processes.
What happens to children who learn or don’t learn about their origins?
Interestingly, children do not seem to be harmed if disclosure does not take place.
Warm parent-child relationships and positive child development have been documented, although few of these donor embryo-conceived children have yet entered adolescence (Golombok S, et al. 2006). While more data and follow up studies are certainly needed, embryo donation children do not seem to be at increased risk for developing psychological problems during early and middle childhood, regardless of disclosure decisions. Supporting these findings about early disclosure, neither the children nor the family seem to be harmed (MacCallum F, et al. 2007 & 2008). While not definitive, the research we have so far suggests that disclosure decisions, either for or against, will not cause irreparable harm to the embryo donor-conceived individuals or the parents who raised them.
Interestingly, research shows that embryo donation families are more child-centered than adoptive and, even, other IVF families, regardless of their disclosure status (MacCallum F, et al. 2007 & 2008). This may be due in part to the recipients’ older age and maturity compared to younger IVF and adoptive parents. Embryo donation-conceived children are tremendously appreciated, greatly desired and hard fought for by their parents. This should give embryo donors confidence that donor-conceived offspring will be well cared for by wonderful recipient families.
What should be considered if embryo donor-conceived individuals meet the donors?
If donor-conceived individuals connect their donors and/or blood siblings, it is important that everyone’s expectations be reasonable. Members of donor-linked families may have a significant mismatch regarding their levels of hope and expectation about contact (Scheib JE, et al. 2008). Some of the participants may have a tendency to romanticize the first meeting and future relationship. The participants should move slowly and carefully, without inappropriate expectations.
It is exceedingly important that the relationship between the parents who raised the child and the embryo donor-conceived offspring not be harmed, as this is the basis for the child’s stability and home life. The fear that this relationship will be damaged is one of the main reasons recipients prefer to not disclose, so it must be protected.
Long-term data regarding the relationships between embryo donors and embryo donor-conceived individuals is not yet available, so we simply are unable to tell any of the participants what the outcome may be (Grotevant HD, et al, 2008). The parents who raised the donor-conceived child may feel threatened by the relationship between the donors and offspring. It would be irresponsible for us as clinicians to assume that all will go well. We must remain cautious and counsel our patients carefully and individually until we have more information to guide them.
Can recipients get help in deciding if disclosure should take place?
Consultation with a mental health professional (MHP) regarding disclosure is strongly encouraged but the counselor must understand the subtle differences between embryo donation and adoption, where disclosure is the norm. Neutrality is required and finding a skilled and experienced MHP is important. Many patients resent direct suggestions about disclosing and far prefer a discussion that examines their own needs and perspectives (Klock SC, 1997). In reality, it is really not appropriate to give a uniform recommendation that does not take into account the personal, ethical and religious views of the embryo recipients.
Even more important, embryo recipients may want to hear from other recipients, people who have worked through the issues or are struggling with making the decision (Klock SC, 1997).
In our three recent surveys examining the perspectives of potential embryo donors, recipients and offspring, there were a few consistent findings:
- From the embryo donor perspective, the majority polled desired an open process.
- From the embryo recipient perspective, the majority polled desired anonymity.
- The majority of potential embryo donors and embryo recipients would disclose to their friends and family.
- If open-identity was available, the majority felt information should be shared and potential contact be made before the age of 18, which may differ in adoption proceedings.
Are reproductive facilities prepared for disclosure?
A medical providers’ first reaction will be to protect their patients: the embryo donors and recipients. State and federal statutes protect confidentiality and clear consent must always be provided before medical/identifying information is released to a third party. The reproductive facilities also will want to be insulated from any legal consequences should disclosure occur.
Some medical practices will be operationally challenged to have records available years after procedures are performed. Many states require that medical records be retained for seven years. The Federal Drug Administration (FDA) requires practices to retain for ten years the medical records of patients involved in third party conception, while the ASRM suggests the records be stored indefinitely. Being able to identify those particular charts from others that would otherwise routinely be discarded is a logistical challenge. In my practice, we color-code the charts involving any type of donor material, making them easy to pull and save.
I also feel embryo recipients have a responsibility to keep the information they were originally provided about their embryo donors protected and safe in case the practice’s medical records are ever lost or deleted.
Regardless, the facilities have a responsibility to assure charts are available and that systems are in place to make disclosure possible. Policies and procedures will need to be created so that they are ready when the requests come. Mirroring the adoption world in this instance may be of use.
How do recipients disclose?
Experienced MHP’s can provide invaluable assistance in helping embryo recipients present this  sensitive information. Reproductive endocrinologists, well versed in this topic, may also be very useful in deciding how and when to tell the children. Forums where parents can discuss these issues with other parents who have lived them also may be indispensible. While few books exist on the topic, I will be reviewing one quite soon that does. Please stay tuned.
sensitive information. Reproductive endocrinologists, well versed in this topic, may also be very useful in deciding how and when to tell the children. Forums where parents can discuss these issues with other parents who have lived them also may be indispensible. While few books exist on the topic, I will be reviewing one quite soon that does. Please stay tuned.
Using the following phrases and ideas in the discussion may be useful:
- We wanted you to be in our lives so much, we had to travel far and wide to find you.
- The people who gave us their embryos, which included you, gave us the most wonderful gift in the world. They loved you so much that they wanted you to enjoy life with us.
- I got to carry and protect you, giving you all the love I could.
- Remember that eggs, sperm and embryos don’t make a family any more than bricks make a happy home. What makes a family is how we support and love each other.
A good way to start this conversation is by emphasizing love, your commitment to find them, the amount of time, effort and emotion you invested in bringing them into the world, and the fact that genetics doesn’t necessarily make a family. I’m sure MHP’s will offer recipients some great phrases and ideas, which I will encourage that they share with us on this blog.
What are the long-term consequences of disclosure?
Research is needed to find out more about long-term disclosure outcomes. It is difficult to ascertain how children are fairing who are not told about their origins fare because these individuals are not readily accessible to research. Also, what happens over time with open donation is largely unknown. I feel it is unrealistic to assume that everyone will live together as one big happy family. I suspect, however, that the donor-conceived children will benefit in establishing connections with blood siblings.
If disclosure occurs and the offspring are destined to contact their genetic parents, their reunion should not be romanticized. They will not necessarily be welcomed with open arms up to two decades later by the donors. In fact, we don’t have any idea how well or how disruptive these reunions will be. Once again, research is desperately needed.
Is there a disclosure compromise available?
The idea of open-identity is a fascinating concept for embryo donation. This would allow donors to be contacted if the recipients eventually disclose the genetic origins to their donor-conceived offspring. According to our recent surveys, most respondents wanted disclosure with open-identity to occur before the children turn 18 and have the ability to contact the donors. But what harm will come to the child if disclosure and contact are done earlier in the formative years? Would there be some advantages to knowing earlier rather than later in adulthood?
It would seem that if recipients are disclosing for the sake of the child, it may truly be best to allow disclosure and open-identity earlier rather than later. I hope to pose this question to MHPs in the months to come.
In summary
I feel it is far better that we design programs with open-identity options but not legislate them. Legislation, especially if it is retroactive, will inject uncertainty about every current rule governing the practice of egg/sperm/embryo donation (Guido P, 2001). Legislation will do more to shut donation processes down than any other development. I understand there are some donor-conceived individuals who feel that all information should be open to review, but past contracts were doubtfully formulated that way. Although unpopular with some, the perceived rights of the donor offspring should not be allowed to circumvent the true legal rights of the donors and recipients.
At a recent ASRM meeting, some MHPs and reproductive attorneys lamented that anonymous embryo donations are allowed to continue. I explained that if they want to change physicians’ and patients’ perspectives on anonymity, they would only succeed with data showing the long-term benefits of disclosure. Until that time, clinicians and patients alike will be hesitant to adopt a stance that is not yet supported by unbiased research. We should tread lightly and make very few assumptions when it comes to issues so important as disclosure or we risk doing harm to our patients. We all need a bit more information in caring for our embryo donors and recipients. We must never forget, however, that embryo donation-conceived individuals, who were never our actual patients, and are still owed thoughtful care and tremendous compassion. We must keep an open mind and learn from their perspective.
There will always be a group of patients who will want anonymity and we all need to respect their wishes. Everyone involved in this debate needs to take a breath and step back. I grow weary of a very vocal group of patients who believe their way is the single right way. This is not a black and white issue. We should instead see the disclosure controversy in shades of grey. Compromise these days seems to be viewed as form of weakness in our country’s politics. This country was founded on the basis of choice and I feel strongly that we should design systems that will allow for choice while educating the participants of embryo donation about their options and the potential results of both disclosure and non-disclosure to embryo donor-conceived individuals. It is our responsibility.
As always I welcome a respectful dialogue, especially from those who disagree. I look forward to reviewing research studies that will guide all of us so we may better counsel embryo donors, embryo donor recipients and especially the embryo donor-conceived individuals, who remain the final focus of this entire discussion.
Craig R. Sweet, M.D.
Reproductive Endocrinologist
Founder, Medical & Practice Director
Embryo Donation International
Info@EmbryoDonation.com
www.EmbryoDonation.com
Associated Blog Segments:
- Introduction: Disclosure Issues in Embryo Donation
- Embryo Donor Perspective
- Survey Results: Imagine you are an Embryo Donor
- Blog: Disclosure Issues From the Perspective of the Embryo Donor (Part 1 & Part 2)
- Embryo Recipient Perspective
- Survey Results: Imagine you are an Embryo Recipient
- Blog: Disclosure Issues From the Perspective of the Embryo Recipient (Part 1 & Part 2)
- Embryo Donor Offspring Perspective
- Survey Results: Imagine you are an Embryo Donor Offspring
- Blog: Disclosure Issues From the Perspective of the Embryo Donor Offspring (Part 1 & Part 2)
Registry Links:
- The Donor Sibling Registry: https://www.donorsiblingregistry.com/
- UK Donor Link: http://ukdonorlink.org.uk/ (funding uncertain)
- Western Australia’s Voluntary Register for Donors, Offspring and their Families: http://www.voluntaryregister.health.wa.gov.au/home/
- BCdonorconception, British Columbia donor offspring: http://groups.yahoo.com/group/BCdonorconception/
Donor Sperm Facility Registries:
- California Cryobank’s Sibling Registry: http://www.sibling-registry.com/
- Fairfax Cryobank: Donor Sibling Groups: http://www.donorsiblinggroups.com/Home_Page.html
General Third Party Conception Support:
- Donor Conception Support Group: http://www.dcsg.org.au/
- PCVAI, People Conceived via Donor Insemination: http://groups.yahoo.com/group/PCVAI/
- International Donor Offspring Alliance: http://www.idoalliance.org/
- The Donor Conception Support Group of Australia Inc: http://www.clan.org.au/dcsg/index.html
- Canadian Donor Offspring: http://www.canadiandonoroffspring.ca/
- Germany: http://www.spenderkinder.de/
References:
Beeson DR, Jennings PK, Kramer W. Offspring searching for their sperm donors: how family type shapes the process. Hum Reprod. 2011 Sep;26(9):2415-24.
Daniels K. The controversy regarding privacy versus disclosure among patients using donor gametes in assisted reproductive technology. J Assist Reprod Genet. 1997 Aug;14(7)-373-5.
De Jonge C, Barratt CL. Gamete donation- a question of anonymity. Fertil Steril. 2006 Feb;85(2)-500-1.
Klock SC. The controversy surrounding privacy or disclosure among donor gamete recipients. J Assist Reprod Genet. 1997 Aug;14(7)-378-80.
Ethics Committee of the American Society for Reproductive Medicine. Informing offspring of their conception by gamete donation. Fertil Steril. 2004 Sep;82 Suppl 1-S212-6.
Ethics Committee of the ASRM. Informing Offspring of their conception by gamete donation. Fertil Steril 2004;81(3):527-31.
Golombok S, Lycett E, MacCallum F, Jadva V, Murray C, Rust J, Abdalla H, Jenkins J, Margara R. Parenting infants conceived by gamete donation. J Fam Psychol. 2004 Sep;18(3):443-52
Golombok S, Murray C, Jadva V, Lycett E, MacCallum F, Rust J. Non-genetic and non-gestational parenthood: consequences for parent-child relationships and the psychological well-being of mothers, fathers and children at age 3. Hum Reprod. 2006 Jul;21(7):1918-24.
Grotevant HD, Wrobel GM, Von Korff L, Skinner B, Newell J, Friese S, McRoy RG. Many Faces of Openness in Adoption: Perspectives of Adopted Adolescents and Their Parents. Adopt Q. 2008 Jul 1;10(3 & 4):79-101.
Guido P. The reduction of sperm donor candidates due to the abolition of the anonymity rule: Analysis of an argument. J Assist Reprod Genet. 2001 Nov;18(11)-617-22.
Jadva V, Freeman T, Kramer W, Golombok S. The experiences of adolescents and adults conceived by sperm donation: comparisons by age of disclosure and family type. Hum Reprod. 2009 Aug;24(8):1909-19.
Klock SC. The controversy surrounding privacy or disclosure among donor gamete recipients. J Assist Reprod Genet. 1997 Aug;14(7)-378-80.pdf
MacCallum F, Golombok S, Brinsden P. Parenting and child development in families with a child conceived through embryo donation. J Fam Psychol. 2007 Jun;21(2):278-87.
MacCallum F, Keeley S. Embryo donation families: a follow-up in middle childhood. J Fam Psychol. 2008 Dec;22(6):799-808.
Mahlstedt PP, LaBounty K, Kennedy WT. The views of adult offspring of sperm donation: essential feedback for the development of ethical guidelines within the practice of assisted reproductive technology in the United States. Fertil Steril. 2010 May 1;93(7):2236-46.
Ravitsky, V. & Scheib, J.E. (2010). Donor-conceived individuals’ right to know. Hastings Center Bioethics Forum 2010;40:(4).
Scheib JE, Ruby A. Contact among families who share the same sperm donor. Fertil Steril. 2008 Jul;90(1):33-43.
Shehab D, Duff J, Pasch LA, Mac Dougall K, Scheib JE, Nachtigall RD. How parents whose children have been conceived with donor gametes make their disclosure decision: contexts, influences, and couple dynamics. Fertil Steril. 2008 Jan;89(1):179-87.
Widdows H, MacCallum F. Disparities in parenting criteria: an exploration of the issues, focusing on adoption and embryo donation. J Med Ethics 2002;28:139-42.
11 Responses to “Disclosure Issues in Embryo Donation: Summary Comments”
-
Dr. Sweet,
This is an excellent, well thought out post about embryo donation! In my opinion, embryo donation is an underused source of third party ART that could benefit so many recipients that long for children, and is a perhaps ethically preferable option for the genetic parents at whose request the embryos were created.
As you point out, disclosure is an important and complex issue with respect to the mental health of the donor-conceived children. In my opinion, another issue worth discussing is whether there ought to be ongoing disclosure requirements related to the ongoing health issues of the genetic parents so that the donor conceived children and their families can take appropriate steps.
-
Craig
A fascinating read and you address quite a few meaty issues affecting more and more people.
The situation is different in the UK as embryo donors used in treatment after April 2005 can be identified by the offspring once they turn 18. However there is no obligation to disclose and it’s hard to tell how many nowadays do. The majority of the research on disclosure is from before removal of anonymity and it might well that the changed landscape of gamete donation in the UK has had a positive impact. Contrary to popular belief pre 2005, sperm and egg-donor numbers actually INcreased after removal of anonymity and there is more open and positive debate.
We are trying to increase embryo donation but it’s a challenging issue. Different ‘types’ of embryo donation require different types of mandatory counselling and managing and most clinics are just not up for that. Understandably; it’s a hugely sensitive and complex issue. Furthermore, there are still some legal loopholes with regards to parenting and no one seems to be in rush to resolve it. http://www.hfea.gov.uk/1972.html
It would be great if we can learn from each other. It’s complex, an ethical minefield, emotionally challenging but more than anything it’s a road worth exploring. There are too many patients waiting for this unique chance and too many donors who, I believe, would want to help if only they knew how.
Laura Witjens
Chair of the National Gamete Donation Trust -
I just want to pick up on one point this time and that is about interaction before the age of 18. One argument is that the security a person has about the family relationships – or indeed the donor conception parents – is likely to be stronger than at say 10. Having said that there are cases where the eldest of donor conception children has the identity of the donor confirmed which will filter through to the younger children of same family.
Another point is when embryos have been used from previously successful treatments. The social and genetic child of the donors will then have to deal with a genetically identical but socially unconnected person wanting to interact with its parents. A tricky scenario and one we would have to be mindful off. As an identifiable donor myself I know my own daughter’s concern, then at the age 9 or 10, that ‘they may want to steal Mummy’. By the time she’s 16 I’m sure it will be more balanced and less threatening.
The children of donor’s are an often overlooked group and whilst I don’t want to create another level of complexity we have to keep in mind they are part of this too.
-
My husband and I have always been open to friends and family about our daughter, who is a 7 year old Donor Embryo baby. She’s incredibly smart, well rounded, and overwhelmingly loved. It’s always been our intent to tell her everything about the amazing journey that we were on to create our family. We often talk about “adopted kids” and how loved they are… she’s fully aware that it took us years to have her, and that included several different doctors in multiple cities – and that we were “always looking for her.” We even have the “Before you were born” and the
The problem is that my daughter suffers from significant separation anxiety. She’s VERY attached to me, and is always concerned that “something bad” is going to happen to me. (Dad travels quite frequently, so I’m often a “single parent”!) When we took her to therapy, the Doctor recommended that we delay telling her about being a DE baby, because of the additional fear of abandonment that it might cause.
So, that leads me to two questions:
1) Do you think that delaying telling her will cause “more harm than good”… assuming that we still continue to address some of the “surrounding factors” of her journey to us? I’m still set on telling her ASAP, but I sure don’t want her panicking that she’s going to be sent or “given back” to strangers.
2) How do I tell doctors that need to know her medical history, and ask them to keep it private – so that they don’t blurt something out to her?? I have some difficult medical forms that require “family history” that I just don’t have, and I don’t think that lying to the doctors will do her any service either.Thanks in advance!
Mini
-
Dear Mini –
I smile when I read letters from parents like yourself. You are incredibly in tune with your child and are clearly looking out for your daughter’s best interest.
Being a mother via egg donation to an amazing son who is 11 years old I can tell you most assuredly that telling your child early and often is not only healthy, but really at the end of the day it’s the right thing to do.
While I am not a psychologist I am the founder and lead an organization (Parents via Egg Donation) that works with parents on a daily basis who grapple with this very situation.I disagree with your psychologist who feels delaying telling your daughter about being a DE kid is the better thing to do and here’s why.
(Now I am not a psychologist – but this has been my experience) – My guess is your daughter’s separation anxiety has zero to do with her DE origins. The fact that your husband travels frequently and you are her sole sense of support, her one and only right now, has probably way more to do with her separation anxiety than the fact she’s a DE kid. When separation anxiety occurs after the age of 6 its most commonly known as a separation anxiety disorder ( I know, I had it as a kid).
What we do know about SAD is that it develops after some sort of big stressor or some kind of trauma a child’s life – like a death of a family member, or a pet, maybe a stay in the hospital, changing schools, moving, etc… I know that being a mother of an only child I fight each and every day of being a helicopter parent (being over protective) and I used to worry that I’d cause my child SAD because of my worry. I had to look long and hard at my own SAD.So not to turn this into a mini psych session, but there is a really great therapist by the name of Carole Lieber Wilkins who not only an amazing therapist she really has made great strides in helping parents talk to their kids about their origins.
To answer your question, waiting I think is not a great idea. I think you can tell your child her story in such a way that not only is she going to feel special (because she is) but she’s going to bond with you even more than she has now. PVED has two great books that I’d be willing to send to you free of charge if you want to email me your address. One is called “One more giraffe” by Kim Noble, and the other is called “Birds of a different feather” by Kelley Wendell. Both are DE mom’s with DE kids, and these are great kid books to share with your daughter about how she came to be.
How do you tell doctors that need to know her medical history to keep it private? I’d just tell any physician that you see that your child is via egg donation and that needs to be kept confidential. Supply that physician with the medical history they need to treat her appropriately, (basically your husbands and the donor’s medical history) and leave it at that.
I apologize for turning this into a novel, but I do want you to know you aren’t alone, there are literally thousands of other parents like you who have amazing children via egg donation. Our organization – PVED (www.pved.org) provides support and education for parents all over the world in any stage of the process.
Warmly,Marna Gatlin,
Founder, Parents via Egg Donation
http://www.pved.org
503 987 1433
marna@pved.org
-
-
[…] of my somewhat long, but comprehensive reviews on the topic by visiting my embryo donation blog by clicking here. This entry was posted in Gamete, Gamete Donation and tagged Dr. Sweet, egg donation, Egg […]
-
[…] of my somewhat long, but comprehensive reviews on the topic by visiting my embryo donation blog by clicking here. This entry was posted in Embryo Donation, Gamete, Gamete Donation, Medical Ethics and tagged […]
Connections at ASRM 2011 Summary
One of the most enjoyable aspects of attending a large professional meeting like the American Society for Reproductive Medicine Annual Meeting is connecting with colleagues, many of whom I had not yet met in person but had gotten to know virtually either via email or through social media.
Some of the highlights of this year’s conference include several delighting conversations and discussions with the following thought leaders in the infertility field:
Mikki Morrissette:
It was a pleasure to meet Mikki at ASRM. We discussed the potential option of having members of the Choice Mom community be able to donate directly to other Choice Mom members in either an open or anonymous fashion. While the details need to be worked out, I can’t help but think that the option is there for this group and others who would desire the same.
Barbara Collura
Executive Director of RESOLVE: The National Infertility Association
http://www.resolve.org/about/barbara-collura-executive-director.html
Barb knows everything and everyone about infertility. She is the go-to-person for all issues involving infertility patient advocacy. As always, it was a pleasure and a learning experience in speaking to her. If I need to know what is really going on, she is the person I ask. I think we will be working quite closely together in the months to come and I know I will learn a tremendous amount from her.
Dawn Gannon
Chair-Elect at ASRM Women’s Council
Professional Outreach Manager at RESOLVE: The National Infertility Association
http://www.linkedin.com/profile/view?id=25083876&locale=en_US&trk=tyah
Having spent time with Dawn at other meetings, she is consistently engaging and knowledgeable and always has a smile on her face. She was one of a few women that I knew at the ASRM Women’s Council meeting, where I truly felt like the odd duck out. I know I will see her at other meetings and it is always enjoyable to spend a few moments with her.
Megan Fabian
Manager, Development and Outreach, Nightlight Christian Adoptions
www.Nightlight.org
Sitting next to Megan during the discussion regarding the personhood amendment was an interesting experience. Understanding that Nightlight is a pro-life organization, I winced a few times as speakers spoke about such individuals with condemnation. Understanding that this is a free society, I feel we should embrace their views as we equally embrace the views offered by pro-choice individuals. In speaking with her afterwards, I think Megan saw, perhaps for the first time, why some of us are so very concerned with using the phrase “embryo adoption,” understanding that assigning personhood to embryos would result in a host of unintended consequences that have the potential to change so much in the world of infertility and women’s healthcare. Even though EDI is not faith-based, we clearly had more in common than not in our united desire to reduce the number of cryopreserved embryos discarded or abandoned and building families whenever we can.
Dawn Davenport
http://www.creatingafamily.org/
Dawn is the executive director of Creating a Family, a nonprofit providing a tremendous amount of educationand support for infertility and adoption. While I had the pleasure of interacting with her online, this was my first opportunity to meet her. She is lovely, very bright and quite tall (I say that of many women as I am only 5’7″ on a good day). EDI may very well work closely with her in the future as we all try to decrease the number of cryopreserved embryos discarded or abandoned while “creating a family” where one would otherwise have not existed.
Amy Demma, Esq.
http://www.lawofficesofamydemma.com/
I wish I had a chance to spend a bit more time with Amy as we were both so very busy at this recent ASRM meeting. She is the absolute queen of social media and brings a tremendous amount of expertise, energy and enthusiasm to the medium. Perhaps we will have time to connect in San Francisco at the upcoming American Association Assisted Reproductive Technology Attorneys (AAARTA) meeting. She is a gem and has a wealth of knowledge and contacts in the field of reproduction.
Davina Frankhauser, M.A.
This bright and insightful young woman is bringing a much-needed perspective to the world of infertility. She and Sandra O’Keefe founded Fertility within Reach™,which serves as an educational resource to increase access to ART for those who need it. I believe as a field, we will find her knowledge and connections invaluable in advocating for infertility awareness and equality as we protect the rights of the infertile patient while facing off against those that believe the infertile patient is utterly expendable as they push for the personhood of embryos.
Judy Weiss, R.N.C.
Judy is a “mench,” a doer of good deeds. As a previous egg donor nurse coordinator who has decades of infertility counseling experience, her clear goal is to help find Jewish egg/sperm donors and surrogates for Jewish families. Understanding that many embryo donation centers are faith-based and frequently aligned with Christianity, she understood the ultimate value of Embryo Donation International. Since we are not faith-based and non-discriminatory, and a potential source of donated embryos with Jewish ancestry, she is excited to offer potential recipients our program. In addition, for those Jewish families who have excess cryopreserved embryos, we will provide a conduit to embryo recipients with similar heritage. I can tell we are going to get along great and work together creating families who would otherwise not exist.
Robert L. Klitzman, M.D.
Columbia University College of Physicians and Surgeons
http://www.amazon.com/Robert-Klitzman/e/B001H9TTMI/ref=ntt_dp_epwbk_0
http://en.wikipedia.org/wiki/Robert_Klitzman
http://asp.cumc.columbia.edu/facdb/profile_list.asp?uni=rlk2&DepAffil=Psychiatry
It was interesting that the two of us showed up to the Legal Professional Group meeting, for which we are both members though neither of us are in the legal profession. Robert and I hit it off a couple of ethical dilemmas as we walked to another meeting. I was envious to learn that he had the opportunity to earn his master’s degree in medical ethics. Upon returning home, I soon discovered the number of books he has
written and can’t wait to pour over them. I can’t help but think we have a great deal in common and look forward to getting his input on a host of issues involving embryo donation and reproductive medicine.
Kathryn Kaycoff-Manos
Co-founder, Global IVF
http://www.globalivf.com/
It was lovely chatting with Kathryn Kaycoff-Manos, one of the directors of Global IVF, a Web resource for infertility consumers from all over the world who are looking for information about infertility treatment in
foreign countries. This can mean Americans looking for more affordable treatment options, especially for third party alternatives, as well as people from Europe, South America and Asia who must seek treatment elsewhere because of legal and accessibility restrictions in their home country. I am excited about the potential of collaborating with Global IVF on the international aspects of Embryo Donation International.
2 Responses to “Connections at ASRM 2011 Summary”
-
Thank you Dr. Sweet for your very kind words. I am honored you would include me/Fertility Within Reach with such a wonderful group of individuals. I must say, the respect you communicated is mutual. It was an absolute pleasure getting to know you and learning what you have accomplished for the infertility community through your practice and Embryo Donation International. Many thanks and congratulations!
Your experiences have left you with sharp instincts. I am hopeful for your future and look forward to staying in touch and connecting again at future ASRM meetings.
All my best,
DavinaDavina Fankhauser, M.A.
President
Fertility Within Reach
http://www.fertilitywithinreach.org -
Why thank you for the inclusion. My head grew a bit by being in such an august group. It was a pleasure meeting you as well. I agree that the human connections are the best part of ASRM.
Part 2: Disclosure from the Perspective of the Embryo Donor Offspring
This is Part 2 of the Disclosure From the Perspective of the Embryo Donor Offspring series. If you missed Part 1 and want to catch up, please scroll below or click here.
How Should Embryo Donor Offspring be Told About Their Origins?
 I wrote in the third segment of this blog series about the best time to disclose genetic identity to embryo donor offspring. I believe that disclosing this information before children are ten years of age may be far better than waiting until they are older, which significantly increases the probability they might be unsettled with the information (Mahlstedt PP, et al. 2010). One of the interesting themes in our surveys has been the consistent finding that the vast majority of respondents would want to know about their origins before age 12 with 91% (10/11) certainly before the age of 18. If Open-Identity were to be practiced in embryo donation, connections between the offspring and the donors may best occur far earlier than what is currently seen with adoption.
I wrote in the third segment of this blog series about the best time to disclose genetic identity to embryo donor offspring. I believe that disclosing this information before children are ten years of age may be far better than waiting until they are older, which significantly increases the probability they might be unsettled with the information (Mahlstedt PP, et al. 2010). One of the interesting themes in our surveys has been the consistent finding that the vast majority of respondents would want to know about their origins before age 12 with 91% (10/11) certainly before the age of 18. If Open-Identity were to be practiced in embryo donation, connections between the offspring and the donors may best occur far earlier than what is currently seen with adoption.
Experienced mental health professionals may prove invaluable in helping parents present this sensitive information. Reproductive endocrinologists well versed in this topic may also be very useful in deciding how and when to tell children. Forums where parents can discuss these issues with other parents who have experienced them may also be indispensible.
I soon will be reviewing a children’s book on this very topic, sharing my thoughts about it with my readers. So stay tuned.
What are the Long-Term Consequences of Disclosure?
Members of donor-linked families may have a significant mismatch regarding their levels of hope and expectation about contact (Scheib E, et al. 2008). Some of the participants may have a tendency to romanticize the first meeting and subsequent relationship. My simple recommendation at this time is to move slowly and carefully, without inappropriate expectations.
It is exceedingly important that the relationship between the parents who raised the child and the embryo donor offspring not be harmed, as this is the basis for the child’s stability and home life. The fear that this relationship will be damaged is one of the main reasons recipients prefer to not disclose.
Remember that little is known about long-term consequences following disclosure and the subsequent contact between embryo donor offspring and their genetic parents and siblings. The complex emotional interplay between embryo donor offspring and the parents who raised them, the embryo donors and the offspring’s genetic is completely unknown. This area of research is sorely needed.
In our most recent survey, 68% of the respondents would tell immediate family, their own children and their significant partners about their embryo donation origins. The only hesitancy involved friends with 40% (4/10) stating that they would not disclose. Once again, the long-term consequences of disclosure remain uncertain with some societies and religions perhaps being less than welcoming to an embryo donation-conceived individual. It would be irresponsible for us as clinicians to assume that all will go well. We must remain cautious and counsel our patients carefully and individually until we have more information to help guide them.
Will the Embryo Donor Offspring Be Hurt by Not Being Told?
Studies that have specifically examined the psychological well being of embryo donation offspring indicate that embryo donation families, independent of disclosure decisions, are faring well (MacCallum F, et al. 2007 & 2008). Warm parent-child relationships and positive child development have been documented although few of these donor embryo-conceived children have yet entered adolescence (Golombok S, et al. 2006). While more data and follow up studies are certainly needed, embryo donation children do not seem to be at increased risk for developing psychological problems during early and middle childhood, regardless of disclosure decisions. The children that were not told of their origin were do as well as those who were told.
Children whose parents do not tell them about their embryo donor origin cannot suffer from lack of disclosure. Whether the parents tell or not, there is research to show that embryo recipient parents may be more attentive and warm to their offspring than natural conception parents.
While not definitive, the research we have so far suggests that disclosure decisions, either for or against, will not cause irreparable harm to the embryo donor-conceived individuals or the parents who raise them.
Summary Comments
Currently, the legal rights of embryo donors and recipients override the strong desire of embryo donor offspring to learn more about or even meet their donors. There is a push to mandate disclosure, but the consequences in the world of embryo donation may be dire. It is quite likely that more embryos will be discarded or abandoned before donors will be forced into an open-identity process.
Using terms such as “mother” and “father” for those who raised the embryo donor offspring should be maintained. The terminology that is used to describe the embryo donors can get confusing. It is my personal choice, but “donor mom ” and “donor dad” seem the simplest and kindest to all.
Reproductive facilities need to prepare for disclosure requests and adhere to record retention guidelines, whenever possible, to avoid unfortunate lapses in information and potential legal consequences.
I understand a donor-conceived individual’s strong desire to know more about their donors. I believe that providing the donor’s medical, surgical, psychiatric, family and social histories is quite reasonable when disclosure occurs. However, providing actual identifying information needs to be handled carefully and thoughtfully. Impartial research to examine the long-term consequences of open-identity issues in embryo donation is sorely needed.
Since physicians take an oath to cause no harm, we all need a bit more information and guidance in caring for our patients, embryo donors and recipients. We must never forget, however, the embryo donation-conceived individuals, who were never our patients, are still owed thoughtful care and tremendous compassion. We have much to learn from them.
References:
Beeson DR, Jennings PK, Kramer W. Offspring searching for their sperm donors: how family type shapes the process. Hum Reprod. 2011 Sep;26(9):2415-24.
Daniels K. The controversy regarding privacy versus disclosure among patients using donor gametes in assisted reproductive technology. J Assist Reprod Genet. 1997 Aug;14(7)-373-5.
De Jonge C, Barratt CL. Gamete donation- a question of anonymity. Fertil Steril. 2006 Feb;85(2)-500-1.
Klock SC. The controversy surrounding privacy or disclosure among donor gamete recipients. J Assist Reprod Genet. 1997 Aug;14(7)-378-80.
Golombok S, Murray C, Jadva V, Lycett E, MacCallum F, Rust J. Non-genetic and non-gestational parenthood: consequences for parent-child relationships and the psychological well-being of mothers, fathers and children at age 3. Hum Reprod. 2006 Jul;21(7):1918-24.
Guido P. The reduction of sperm donor candidates due to the abolition of the anonymity rule: Analysis of an argument. J Assist Reprod Genet. 2001 Nov;18(11)-617-22.
MacCallum F, Golombok S, Brinsden P. Parenting and child development in families with a child conceived through embryo donation. J Fam Psychol. 2007 Jun;21(2):278-87.
MacCallum F, Keeley S. Embryo donation families: a follow-up in middle childhood. J Fam Psychol. 2008 Dec;22(6):799-808.pdf
Mahlstedt PP, LaBounty K, Kennedy WT. The views of adult offspring of sperm donation: essential feedback for the development of ethical guidelines within the practice of assisted reproductive technology in the United States. Fertil Steril. 2010 May 1;93(7):2236-46.
Ravitsky, V. & Scheib, J.E. (2010). Donor-conceived individuals’ right to know. Hastings Center Bioethics Forum 2010;40:(4).
Scheib JE, Ruby A. Contact among families who share the same sperm donor. Fertil Steril. 2008 Jul;90(1):33-43.
Shehab D, Duff J, Pasch LA, Mac Dougall K, Scheib JE, Nachtigall RD. How parents whose children have been conceived with donor gametes make their disclosure decision: contexts, influences, and couple dynamics. Fertil Steril. 2008 Jan;89(1):179-87.
Disclosure Issues From the Perspective of Embryo Donor Offspring
In an Open Embryo Donation procedure it is likely the embryo donor-conceived individuals will be told of their origin. In an anonymous procedure, however, it is up to the embryo recipient parent(s) to make disclosure decisions. Reproductive endocrinologists are normally focused on the donor’s and the recipient’s legal rights/rights to privacy and we probably loose sight of the offspring’s point of view. These next two segments will examine this potentially neglected perspective: those of the children and adults created through embryo donation.
Do Embryo Donor Offspring Have The Right to Know Their Origins?
 Many donor-conceived person feel they have a perceived right and a strong desire to know their genetic origins (Shehab D, et al. 2008). From an ethical perspective, these individuals feel disclosure of their true genetic origins involves principals such as honesty, trust and respect.
Many donor-conceived person feel they have a perceived right and a strong desire to know their genetic origins (Shehab D, et al. 2008). From an ethical perspective, these individuals feel disclosure of their true genetic origins involves principals such as honesty, trust and respect.
Embryo donors and recipients, who may prefer an anonymous process, seem to have rights that compete with those of the donor-conceived individuals. In reality, both embryo donors and recipients have legal rights that are in direct contrast to the offspring’s moral view that family secrets shouldn’t be hidden.
There is a very vocal and select group of egg and sperm donors who feel disclosure should be mandatory. It should be understood, however, that we are probably not hearing from those embryo donor-conceived individuals who have been told of their origins, but who are less vocal, perhaps feeling that disclosure should not be mandated or legislated. We simply do not know if this is a silent minority or majority.
In many ways, there is no easy way to reconcile these contrasting legal rights and moral perspectives. Most agree, at the risk of offending those who feel differently, that in society ruled by law, that a legal right ultimately trumps a perceived moral right. Thus, the legal rights of donors and recipients continue to prevail in this country.
That stated, if individuals are told they came from donated embryos, it is natural to expect they will want more information.
Why do Embryo Donor Offspring Want Disclosure?
While perhaps not directly comparable, those sperm and egg donor-conceived offspring who are seeking information about their donors often do so for the following reasons (Ravitsky V, et al. 2010 & Mahlstedt PP, et. al. 2010):
- Curious about donor physical characteristics and personalities
- Desire a better understanding of their own genetic identity
- Have medical concerns (medical, family and social history)
- Want to meet the donor
- Want to understand the motivations of the donors
- Want to provide an ancestral history for their own children
For children born to a single woman or a lesbian couple, finding out more about the donors may increase their sense of kinship. Open-identity systems are being driven forward, in part, through single women and lesbian couple donor sperm recipients. These recipients are also the most likely to disclose because their social situation essentially requires it.
For many, the search for their donors may go well beyond seeking just simple information. In two recent studies of offspring searching for their donor sperm fathers, with about half over the age of 18 and half under, between 80-88% were intensely curious about their donor and wanted to contact them. Up to one-third desired an actual relationship with the sperm donor (Beeson DR. 2011 & Bahlstedt PP, et al. 2010). It should be understood, however, that support group studies such as these might not represent a balanced patient sample. Donor offspring who are not bothered by the issue are less likely to seek information/support via the web and are, therefore, not enrolled in such studies. Interestingly, our recent survey on this same topic yielded nearly identical results with 82% (9/11) respondents wanting medical and/or identifying information on their embryo donors.
What do Embryo Donor Offspring Call Their Donors and Recipients?
Here are some terms commonly used to describe embryo donors and embryo donor recipients from the perspective of the offspring who have been told they were created though embryo donation:
|
Embryo Donors |
Embryo Recipients |
|
|
These important labels have emotional connotations and I have listed them here in my personal order of preference.
Are Reproductive Facilities Prepared for Disclosure?
In general, reproductive facilities may not be adequately prepared to handle embryo donation disclosure issues. Medical providers’ first reaction will be to protect their patients, the donors or recipients. Nondisclosure of medical information is actually required by state and federal statutes and clear consent must always be provided before medical/identifying information is released to any third party.
Most reproductive facilities are totally unaware of the adoption literature that universally advocates disclosure. Clinicians will want conclusive embryo donation studies before they will consistently recommend and comply with disclosure. They will also want to be insulated from any legal consequences should disclosure occur.
Most medical practices will be operationally challenged to have records available years after procedures are performed. Most states require medical records to be retained for seven years. The FDA requires charts involved with third party conception techniques to be kept for 10 years, while the ASRM suggests they be stored indefinitely. Being able to identify those particular charts from the others charts is a logistical challenge. In my practice, we color-code the charts involving any type of donor material, making them easy to pull and save.
In the case of natural disasters, paper charts may be destroyed. It is common sense that the medical practice should also save the information in electronic form with offsite back up. Keeping in mind that electronic document formats are constantly changing, we currently suggest documents be saved in the common “pdf” (Adobe Portable Document Format) file format, and keep the medical and identifying information separate.
I also feel embryo recipients have a responsibility to keep the information about their embryo donors protected and safe just in case the practice’s medical records are ever lost or deleted.
We will continue this discussion, on disclosure issues from the perspective of the embryo donor offspring, tomorrow. Included will be discussion of whether or not reproductive facilities are prepared for disclosure, long-term consequences and how to tell the offspring. The reference list will also be posted with the second half. Stay tuned!
Disclosure Issues in Embryo Donation: Part 4 of 5
Brief Introduction
This is the fourth of a five-part series examining the complex decision-making surrounding the disclosure of the genetic origins of embryo donor offspring to family, friends and the offspring themselves. There were 11 respondents with the results examined below.
Associated Blog Segments
The first segment of this series introduced the disclosure topic and our first survey. The second segment (Part 1 and Part 2) examined disclosure issues from the perspective of the embryo donor, incorporating a survey that asked opinions from our readers. The third segment (Part 1 and Part 2) examined disclosure from the perspective of the embryo recipient, including our final survey. The results are discussed below.
Survey Results: “Imagine You Were an Embryo Donor Offspring”
1. Regarding the topic of disclosure of my genetic origins:
| I would not desire to know that I was created through donated embryos. The parents who raised me are simply my parents and it doesn’t really matter if I came from donated embryos. | 18% (2/11) |
| I would like to know all the available medical information about the embryo donors. I would not, however, want identifying information. | 46% (5/11) |
| I would like to know all the available medical information about the embryo donors. In addition, I would like to be provided identifying information. | 36% (4/11) |
Comments:
In this small study sample, the majority [82% (9/11)] wanted to know medical information about their embryo donors, with about half wanting identifying information. These numbers are similar to published data on the desires of egg and sperm donation-conceived individuals.
2. If I were to be told about being an embryo donor offspring, I would want to be told (choose only one):
- Sometime during ages 1-6 years old 55% (6/11)
- Sometime during ages 7-12 years old 18% (2/11)
- Sometime during ages 13-18 years old 18% (2/11)
- After age 18 9% (1/11)
Comments:
The majority [91% (10/11)] would prefer to be told of their embryo donor origins before the age of 18, with most wanting to know at 12 years of age or younger. As I wrote in the previous blog, disclosure to the embryo donor-conceived individual after age 10 tends to result in feelings of mistrust, alienation, identity confusion, frustration and even hostility towards their family (Ethics Committee, 2004 & Mahlstedt PP, et al. 2010).
3. If I were provided medical and identifying information about the embryo donors, I would do the following (choose only one):
| I would not try to contact the embryo donors. | 55% (6/11) |
| I would try to contact the embryo donors but am most interested in learning about and potentially contacting my blood brothers and sisters. | 45% (5/11) |
| I would try to contact the embryo donors to establish a relationship with the genetic parents and my blood brothers and sisters. | 0% (0/11) |
Comments:
About half of those polled would not try to contact the embryo donors while the other half would be interested in contacting their genetic siblings. Published articles on the topic suggest that most donor-conceived individuals are more curious, with many wanting to meet their donors. I believe that if given the contact information, most embryo donor-conceived individuals will become quite curious over time and will eventually want to interact with their genetic siblings and/or the embryo donors themselves.
4. If I found out that I was the product of embryo donation, I would tell the following people:
| Relationship | Yes | No | N/A (not alive or no current relationship) |
| My “significant other” | 91% (10/11) | 0% (0/11) | 9% (1/11) |
| My in-laws | 60% (6/10) | 10% (1/10) | 30% (3/10) |
| My children | 60% (6/10) | 10% (1/10) | 30% (3/10) |
| My friends | 60% (6/10) | 40% (4/10) | 0% (0/10) |
| Average: | 68% (28/41) | 15% (6/41) | 17% (7/41) |
Comments:
If one removes the “N/A” category, which didn’t pertain to some of the poll respondents, the majority of embryo donor-conceived individuals would tell their immediate family about their genetic origin, especially to their “significant other.” It would appear, however, that there was some hesitation to tell their friends the same information.
Tomorrow we will release the next installment of this series – Disclosure Issues From the Perspective of the Embryo Donation Offspring. This will be released in two separate sections with the second half released the day after the first.
Next week, we will release our final summary of this series, combining the perspectives of the embryo donors, embryo recipients and embryo donation-conceived offspring.







[…] Do These Embryos Make the Grade? The details of embryo grading may seem a bit dry, but it is important if you’re going through IVF, and this blog did a good job of explaining the details. It’s a fast and easy read, so don’t be put off by the topic. The blog was written for the embryo donation audience, but the info is equally useful for the average IVF patient, if there is such a thing. Share and Enjoy: […]
Thanks for the comment. It is a bit difficult to make the discussion regarding embryo grading very exciting and anything less than dry. Having patients understand what physicians and embryologists are trying to saying when they are describing the overal grade of their embryos is so very important.
I also agree that the information is useful to anyone undergoing assisted reproductive technologies. Thanks again for the comments and keep them coming!
Craig R. Sweet, M.D.
Reproductive Endocrinologist
If you had to choose between day 5 blasts vs day 6 blasts for et which would you transfer? ( provided both sets were of the same grade/quality ?). Many thanks!