Archive for June, 2011
Human Embryonic Stem Cell Research – Reimbursement Debate
Should Patients be Reimbursed for Donating Their Embryos for Human Embryonic Stem Cell Research?
By Dr. Craig R. Sweet
Medical & Practice Director
Founder, Embryo Donation International
Introduction:
There are a handful of academic and private research facilities in the U.S. performing human embryonic stem cell (hESC) research. The use of embryos for research is an emotionally charged issue, with prolife and prochoice proponents having opposite viewpoints. The advantages and disadvantages of the research are not the focus of this discussion. EDI feels this is a very personal choice, which only should be made with great care and thought.
Let us assume for now, and at the risk of offending some, that there is potential merit to hESC research.
Most Donors Change Their Minds
Approximately 71% of the patients who state they will donate their unused embryos routinely change their minds, with most discarding them instead (Klock SC, et al. 2001). In fact, only about 5-10% of the patients actually donated their unused embryos for hESC research (Elford K, et al. 2004 & Klock SC, et al. 2001). Why do so many change their minds?
Would the percentage of embryos donated for research increase if donors were given a minimum level of financial reimbursement?
Inappropriate Enticement?
Centers performing hESC research are under very strict guidelines. Institutional review boards for human experimentation, which oversee such studies, forbid any level of coercion in obtaining embryos. Coercion can mean many things, including offering excessive financial incentives. But in my opinion, restricting even small tokens of appreciation can be counterproductive. For example, when we worked with Harvard’s hESC lab, we wanted to offer patients a $25 gift card to encourage them to complete the paperwork within 30 days so we could transport the embryos to the study facility as quickly as possible. Soon after starting this, we were told to stop because even a $25 gift card might be interpreted as inappropriate enticement.
Does anyone really think the $25 would inappropriately convince a patient to
donate their embryos for hESC research when they would otherwise not have done so?
In a pilot study performed by our parent organization, Specialists In Reproductive Medicine & Surgery (SRMS), we found the average cost per embryo transferred or cryopreserved was $2,400. This study included patients with and without insurance coverage. These estimates didn’t include the costs of time away from work, pain, suffering or any other infertility treatment expenses leading up to the IVF procedure. Interestingly, the cost per embryo transferred or cryopreserved ranged from $650 to $23,000.
What if the reimbursement was always far less than the amount that was spent to create the embryos, to make certain no one ever created embryos for profit?
Will Researchers Benefit?
Is there any doubt that academic centers and private companies may benefit from hESC research? If there is a scientific breakthrough at a hESC research facility, isn’t it reasonable that they will benefit from research dollars and/or actual profits? Even the American Medical Association’s (AMA) Council on Ethical and Judicial affairs states: “Profits from the commercial use of human tissue and its products may be shared with patients, in accordance with lawful contractual agreements.” (AMA, Opinion 2.08)
Is it wrong to ask why the patients who provided the embryos shouldn’t be reimbursed for even a fraction of what it took to create them?
What Do Patients Think?
In Netwon’s 2003 paper examining attitudes towards embryo donation procedures, 16% of those interviewed rejected embryo donation without some reimbursement with another 32% uncertain. (Newton CR, et al. 2003). This is compelling evidence that some patients felt the embryos had worth and that a level of reimbursement was not only desired, but required.
What Did You Think?
We conducted a poll on Facebook asking: “Should patients be compensated for donating their embryos for human embryonic stem cell research? Why or why not?” The following were the results:
- No: 11 people (69%)
- Uncertain: 2 (12%)
- Yes: 3 (19%)
While not a very large poll, the overriding opinion was no. I certainly respect their view. Clearly, reimbursement is not appropriate for all. I can’t help but wonder, however, if it would be appropriate for some.
I suggest that reimbursement for research studies is commonplace but seems to be forbidden in hESC research. What makes it so different? Facilities conducting this research are under a magnifying glass and most likely are afraid of criticism regarding human embryos. Are they afraid of a public relations backlash? Perhaps they truly feel it is ethically inappropriate, even though participants in other forms of clinical research; sperm, egg, and blood plasma donation; and surrogacy and adoption are reimbursed or compensatedfor reasonable and customary expenses and time and effort. But any suggestions about reimbursing for human embryos seem to be taboo.
Will Reimbursement Reduce the Number of Embryos Discarded?
So will adding a small financial incentive change human behavior and reduce the number of embryos discarded? Would a study exploring this clear institutional review board perusal for human experimentation oversight? Simply posing the question won’t work as people change their minds about embryo disposition. A randomized, multi-center longitudinal study might answer the question. In this study, some patients would be reimbursed and others not, with the number of embryos donated to patients in need or research would be compared to the number that were ultimately discarded.
Will anyone be brave enough to initiate such a study?
In Summary
What if a small amount of money was provided for embryos destined for hESC research? If reimbursement was provided, the research facility would need to require documentation of the money spent to create the embryos. It would be absolutely necessary that the facility always pay far less than it ever took to create the embryos. We must make certain that no one would ever create the embryos for profit, something I feel is overwhelmingly inappropriate.
Those who do not feel comfortable with reimbursement could simply refuse or request a donation be made to charity. Since we currently are forbidden to reimburse patients for embryos donated to patients in need at EDI, we instead donate to charity in either the donor’s name or anonymously. It is the best compromise we could find.
Perhaps fewer embryos would be discarded, abandoned or perpetually cryopreserved if we motivated patients with direct reimbursement or donation to charity. If we did so, might the greater good be served?
References:
Opinion 2.08 – Commercial use of Human Tissue. AMA Code of Medical Ethics.
http://www.ama-assn.org//ama/pub/physician-resources/medical-ethics/code-medical-ethics/opinion208.pageElford K, Lawrence C, Leader A. Research implications of embryo cryopreservation choices made by patients undergoing in vitro fertilization. Fertil Steril. 2004 Apr;81(4):1154-5.
Klock SC, et al. The disposition of unused frozen embryos [letter]. N Engl J Med 2001;345(1):69-70.
Newton CR, et al. Embryo donation- attitudes toward donation procedures and factors predicting willingness to donate. Hum Repro 2003;18(4):878-84.
How Long do Embryos Last?

By Corey Burke, B.S., C.L.S.
Embryologist & Andrologist
Laboratory Supervisor
I am often asked: “How long do frozen embryos last?” The answer to this question is a little more complicated than simply replying with a specific number of years because several factors influence the answer.
question is a little more complicated than simply replying with a specific number of years because several factors influence the answer.
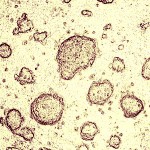
The first successful pregnancy from a cryopreserved (frozen) embryo occurred in 1983 (Trounson A, Mohr L. 1983). Shortly thereafter, embryo cryopreservation became commonplace, with millions of embryos cryopreserved over the past few decades. Recently, a live birth was reported from an embryo cryopreserved for 20 years (Dowling-Lacy D, et al. 2011). There is, however, uncertainty regarding the health of frozen embryos over time. Since embryologists have only been cryopreserving embryos for slightly less than 30 years, it is impossible to know right now if extended storage times much beyond two decades will influence embryo survival and pregnancy rates.
A study that is the largest of its kind was recently published in March 2011. It examined approximately 12,000 cryopreserved embryos, and determined that the length of storage time did not influence post thaw survival rates or the actual pregnancy outcomes (Riggs R, et al. 2010). The embryos in this study had been frozen up to nine years.
 The technique for freezing embryos in liquid nitrogen has changed over time. The original method was known as a “slow freeze” technique, where the temperature of the embryos slowly dropped over a couple of hours. Vitrification, a newer method, freezes the embryos in a minute fraction of a second. While survival rates for embryos frozen through vitrification seem higher, it is uncertain if vitrified embryos will result in more pregnancies (Khoury C, et al. 2010). My guess is there will actually be little difference between the two freezing methods since the embryos end up in the same suspended animation of liquid nitrogen at -196°C (-321° F). If the embryo survives the thaw, pregnancy rates may not depend on the duration of time it was frozen or the technique used to freeze it.
The technique for freezing embryos in liquid nitrogen has changed over time. The original method was known as a “slow freeze” technique, where the temperature of the embryos slowly dropped over a couple of hours. Vitrification, a newer method, freezes the embryos in a minute fraction of a second. While survival rates for embryos frozen through vitrification seem higher, it is uncertain if vitrified embryos will result in more pregnancies (Khoury C, et al. 2010). My guess is there will actually be little difference between the two freezing methods since the embryos end up in the same suspended animation of liquid nitrogen at -196°C (-321° F). If the embryo survives the thaw, pregnancy rates may not depend on the duration of time it was frozen or the technique used to freeze it.
While there clearly are many variables that influence the health and implantation rate of an embryo, the length of storage is probably not one of them. Data still needs to be collected but the information we have so far is encouraging.
As time marches forward, I expect additional cases to be reported that will lengthen the 20-year cryopreservation “ceiling” to decades longer. Amazingly, it is estimated that mammalian cells will last for hundreds or even thousands of years when frozen in liquid nitrogen (Mazur P. 1980). If this is true, these frozen embryos will certainly outlast all of us.
References:
Dowling-Lacey D, Mayer JF, Jones E, Bocca S, Stadtmauer L, Oehninger S. Live birth from a frozen-thawed pronuclear stage embryo almost 20 years after its cryopreservation. Fertil Steril. 2011 Mar 1;95(3):1120.e1-3.
Khoury C, Fredrick J, Behr B, Potter D. A Comparison of Blastocyst Slow Freeze and Vitrification in Frozen Blastocyst Transfer. Fertil Steril. 2010 Mar;93(5): S14-15
Mazur P. Limits to life at low temperatures and at reduced water contents and water activities. Orig Life 1980;10:137–59.
Riggs R, Mayer J, Dowling-Lacey D, Chi TF, Jones E, Oehninger S. Does storage time influence postthaw survival and pregnancy outcome? An analysis of 11,768 cryopreserved human embryos. Fertil Steril. 2010 Jan;93(1):109-15.
Trounson A, Mohr L. Human pregnancy following cryopreservation, thawing and transfer of an eight-cell embryo. Nature 1983;305:707–9.