Author Archive
How Long do Embryos Last?

By Corey Burke, B.S., C.L.S.
Embryologist & Andrologist
Laboratory Supervisor
I am often asked: “How long do frozen embryos last?” The answer to this question is a little more complicated than simply replying with a specific number of years because several factors influence the answer.
question is a little more complicated than simply replying with a specific number of years because several factors influence the answer.
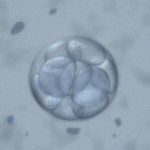
The first successful pregnancy from a cryopreserved (frozen) embryo occurred in 1983 (Trounson A, Mohr L. 1983). Shortly thereafter, embryo cryopreservation became commonplace, with millions of embryos cryopreserved over the past few decades. Recently, a live birth was reported from an embryo cryopreserved for 20 years (Dowling-Lacy D, et al. 2011). There is, however, uncertainty regarding the health of frozen embryos over time. Since embryologists have only been cryopreserving embryos for slightly less than 30 years, it is impossible to know right now if extended storage times much beyond two decades will influence embryo survival and pregnancy rates.
A study that is the largest of its kind was recently published in March 2011. It examined approximately 12,000 cryopreserved embryos, and determined that the length of storage time did not influence post thaw survival rates or the actual pregnancy outcomes (Riggs R, et al. 2010). The embryos in this study had been frozen up to nine years.
 The technique for freezing embryos in liquid nitrogen has changed over time. The original method was known as a “slow freeze” technique, where the temperature of the embryos slowly dropped over a couple of hours. Vitrification, a newer method, freezes the embryos in a minute fraction of a second. While survival rates for embryos frozen through vitrification seem higher, it is uncertain if vitrified embryos will result in more pregnancies (Khoury C, et al. 2010). My guess is there will actually be little difference between the two freezing methods since the embryos end up in the same suspended animation of liquid nitrogen at -196°C (-321° F). If the embryo survives the thaw, pregnancy rates may not depend on the duration of time it was frozen or the technique used to freeze it.
The technique for freezing embryos in liquid nitrogen has changed over time. The original method was known as a “slow freeze” technique, where the temperature of the embryos slowly dropped over a couple of hours. Vitrification, a newer method, freezes the embryos in a minute fraction of a second. While survival rates for embryos frozen through vitrification seem higher, it is uncertain if vitrified embryos will result in more pregnancies (Khoury C, et al. 2010). My guess is there will actually be little difference between the two freezing methods since the embryos end up in the same suspended animation of liquid nitrogen at -196°C (-321° F). If the embryo survives the thaw, pregnancy rates may not depend on the duration of time it was frozen or the technique used to freeze it.
While there clearly are many variables that influence the health and implantation rate of an embryo, the length of storage is probably not one of them. Data still needs to be collected but the information we have so far is encouraging.
As time marches forward, I expect additional cases to be reported that will lengthen the 20-year cryopreservation “ceiling” to decades longer. Amazingly, it is estimated that mammalian cells will last for hundreds or even thousands of years when frozen in liquid nitrogen (Mazur P. 1980). If this is true, these frozen embryos will certainly outlast all of us.
References:
Dowling-Lacey D, Mayer JF, Jones E, Bocca S, Stadtmauer L, Oehninger S. Live birth from a frozen-thawed pronuclear stage embryo almost 20 years after its cryopreservation. Fertil Steril. 2011 Mar 1;95(3):1120.e1-3.
Khoury C, Fredrick J, Behr B, Potter D. A Comparison of Blastocyst Slow Freeze and Vitrification in Frozen Blastocyst Transfer. Fertil Steril. 2010 Mar;93(5): S14-15
Mazur P. Limits to life at low temperatures and at reduced water contents and water activities. Orig Life 1980;10:137–59.
Riggs R, Mayer J, Dowling-Lacey D, Chi TF, Jones E, Oehninger S. Does storage time influence postthaw survival and pregnancy outcome? An analysis of 11,768 cryopreserved human embryos. Fertil Steril. 2010 Jan;93(1):109-15.
Trounson A, Mohr L. Human pregnancy following cryopreservation, thawing and transfer of an eight-cell embryo. Nature 1983;305:707–9.
The Frozen Embryo Dilemma
Are Disposal Ceremonies or Compassionate Transfers the Answer to the Frozen Embryo Dilemma?
By Dr. Craig R. Sweet
Medical & Practice Director
Founder, Embryo Donation International
In recent years, researchers led by Dr. Anne D. Lyerly of Duke University have conducted several studies about infertility patients’ attitudes toward disposition of excess frozen embryos. Their research has shed some light on the difficulties facing patients about this important decision and patient reaction to the different options clinics offer.
As a quick review, options for excess frozen embryos are:
- Personal reproductive use
- Donation to research
- Donation to patients in need
- Thaw and discard
Timing has a significant impact on patient decision-making. Clearly, the in vitro fertilization (IVF) process can  overwhelm patients. First, they’re worried about whether they will create embryos and, then, about how many of them will be high quality. Then after the transfer, they endure the long wait while hoping and dreaming for a positive pregnancy test and an encouraging ultrasound weeks later. The last thought on their mind involves the eventual disposition of excess frozen embryos. It is probably unreasonable to expect patients to make this type of decision, but most fertility clinics ask them to select an option before they even start of the IVF process. Many patients stated that from the start the IVF clinics didn’t do a good job in explaining their choices (Lyerly AD, et al 2008). While this may be true in some instances, clinics may have explained the alternatives well, but patients simply couldn’t absorb all the information. When forced to decide what to do with the cryopreserved embryos before they have successfully delivered a child through IVF and/or have made the decision to stop treatment, many patients will inevitably change their minds.
overwhelm patients. First, they’re worried about whether they will create embryos and, then, about how many of them will be high quality. Then after the transfer, they endure the long wait while hoping and dreaming for a positive pregnancy test and an encouraging ultrasound weeks later. The last thought on their mind involves the eventual disposition of excess frozen embryos. It is probably unreasonable to expect patients to make this type of decision, but most fertility clinics ask them to select an option before they even start of the IVF process. Many patients stated that from the start the IVF clinics didn’t do a good job in explaining their choices (Lyerly AD, et al 2008). While this may be true in some instances, clinics may have explained the alternatives well, but patients simply couldn’t absorb all the information. When forced to decide what to do with the cryopreserved embryos before they have successfully delivered a child through IVF and/or have made the decision to stop treatment, many patients will inevitably change their minds.
It would appear that almost half of all the estimated hundreds of thousands of cryopreserved embryos are not used for reproduction. We found this to be true in our own 2006 internal review and others have published similar statistics. As I have written before, the decision regarding what to do with excess cryopreserved embryos is very difficult such that 15% of the patients choose to not decide and keep their embryos frozen indefinitely (Lyerly AD, et al. 2011).
Many patients don’t like any of the existing alternatives for frozen embryos. A disposal ceremony at the time of thaw and/or a compassionate transfer may be better options. A compassionate transfer occurs when the embryos are placed into a women’s uterus or vagina at a time when she can’t conceive. Some patients prefer this process, letting the embryos be absorbed naturally and allowing closure while honoring what has been described as the physical and emotional attachments between them and their embryos (Lyerly AD, et al. 2006 & 2011). One of the rare studies to examine if patients would choose compassionate transfer found that about 20% would consider this alternative (Lyerly AD, et al. 2010). In a separate but associated article written by the same author in 2011, she stated:
“Given the morally difficult nature of the disposition decision, informed consent is unlikely to be the full solution: ensuring options that patients find responsible and respectful, such as compassionate transfer or a disposal ceremony may benefit those who assign high moral status or value to the embryos but are disinclined to donate them to another couple.”
There are, unfortunately, three problems with these two options. The first is that very few facilities offer these disposal techniques (Gurmankin AD et al. 2004). Second, I can’t help but wonder who is receiving the compassion, the patients (probably) or the embryos? Third, no matter how you phrase it, the embryos are still being thawed and discarded.
Let me be clear that the parent organization of Embryo Donation International (EDI), Specialists In Reproductive Medicine & Surgery, P.A. (SRMS), removed the destruction option for excess frozen embryos years ago, believing that better alternatives existed. I feel the embryos deserve an intermediate level of respect and that donating them to research (human embryonic stem cell or other valuable studies) or donating them to patients in need serve a greater good for the embryos and society as a whole. We try to make this as clear as we can to the patients undergoing IVF at SRMS, emphasizing our non-destruct policy in our consent. Interestingly, over the years, not one patient or couple has disagreed with the policy. Our desire is that other facilities consider what we call our “non-destruct” policy.
EDI/SRMS’ views are currently in the minority, with the majority of IVF programs still allowing patients to thaw and discard their embryos (Gurmankin AD et al. 2004). While I would far prefer that patients consider donation to research or patients in need, as a clinician, I have to be aware that my personal and professional views may differ significantly from others.
Perhaps the facilities that continue to offer the thaw and discard option would consider offering alternatives that some patients really want. It would seem a disposal ceremony consistent with the patient’s religious or spiritual beliefs or a compassionate transfer are two options patients prefer but rarely seem to be able find.
I still implore patients with excess cryopreserved embryos to consider embryo donation and to pay it forward to other infertile patients traveling the difficult infertility road without success. From my perspective, the best option is to take a deep breath and make the difficult decisions that will not result in the discarding of their cryopreserved embryos. If, however, a disposal ceremony or compassionate transfer will result in embryos not being abandoned or frozen forever, then perhaps this is a marginally better option to consider. Marginally better, but still in my mind, not the best of the options readily available.
Craig R. Sweet, M.D.
Founder, Embryo Donation International
Reproductive Endocrinologist
Medical & Practice Director
Excellent References:
– Gurmankin AD, Sisti D. Embryo disposal practices in IVF clinics in the United States. Politics and the Life Sciences. 2004;22(2):4-8.
– Lyerly AD, et al. Decisional conflict and the disposition of frozen embryos: implications for informed consent. Hum Reprod. 2011 Mar;26(3):646-54.
– Lyerly AD, et. al. Factors that affect infertility patients’ decisions about disposition of frozen embryos. Fertil Steril 2006;85:1623-30.
– Lyerly AD, et al. Fertility patients’ views about frozen embryo disposition: results of a multi-institutional US survey. Fertil Steril 2010;93:499-509.
To be discussed in the next blog, please share your opinion.
![]() Loading ...
Loading ...
Safe Travels on Your Infertility Journey
 By Dr. Craig R. Sweet, Medical Director & Founder
By Dr. Craig R. Sweet, Medical Director & Founder
I sit here wondering what I can write about that others will not already be commenting on during this very busy and important National Infertility Awareness Week for those traveling the infertility journey. But after over 20 years of taking care of tens of thousands of patients, I have developed a few philosophical perspectives and “rules of the road” and I want to share with you.
Don’t Wait Until All Your Ducks Are in a Row
First, a woman’s ability to conquer the world does not necessarily transfer to conquering the biologic clock that endlessly ticks forward. My IVF patients already are arriving at my doorstep at an average age of close to 37, which puts them at a significant disadvantage. If I could encourage young women to do anything, it would be to try to start their families earlier. If they wait to have all their “ducks in a row,” they may never see their little ducklings.
Hollywood is rife with women conceiving late in life, but they rarely tell anyone that they used donated eggs, not that it is our business. Please, I implore women around the world to have their children sooner and not depend on our modestly advanced technologies to prevail when nature argues differently.
Seek Knowledge Sooner Rather Than Later
Second, if you are having problems conceiving, see a knowledgeable local reproductive endocrinologist sooner rather than later. Don’t be  pressured to start a more intensive evaluation or procedures one day earlier than you are ready but seek knowledge sooner. Obtain an opinion from someone you trust to see where you stand and to get a glimpse into your reproductive future. At the risk if alienating some referring physicians, do not be satisfied with seeing general OB/GYN physicians or Urologists to seek solid information should problems be found. Knowledge is power; obtain it quickly with experts who live and breath your issues each and every day.
pressured to start a more intensive evaluation or procedures one day earlier than you are ready but seek knowledge sooner. Obtain an opinion from someone you trust to see where you stand and to get a glimpse into your reproductive future. At the risk if alienating some referring physicians, do not be satisfied with seeing general OB/GYN physicians or Urologists to seek solid information should problems be found. Knowledge is power; obtain it quickly with experts who live and breath your issues each and every day.
Don’t Be Afraid of the Unknown
Third, don’t be afraid of what you might find. Take a deep breath and learn the truth. I see far too many patients that fear for too long, only to find out their fears were incorrect, or that their delay significantly impaired their overall chances for success while inadvertently increasing their costs to succeed. Be brave, find support and gain knowledge quickly. Do not be afraid. This is absolutely directed at both the male and female patients.
In Closing
I will leave it up to RESOLVE and many other organizations to do what they do best: organizing patients to speak with one united voice during this very important week. During this week of attention, a philosophical perspective may really be of some benefit hopefully heard among the din of all the other conversations.
Infertility is a journey and what journey should start without a few rules of the road?
Craig R. Sweet, M.D.
Founder, Embryo Donation International
Reproductive Endocrinologist
Medical & Laboratory Director
The Disposition of Cryopreserved Embryos
 By Dr. Craig R. Sweet, Medical Director & Founder
By Dr. Craig R. Sweet, Medical Director & Founder
During in vitro fertilization (IVF), numerous eggs are removed from the woman, and fertilized with sperm to create embryos that are grown in the laboratory for several days. Almost always the final number of embryos available for transfer is less than the number of eggs (oocytes) originally retrieved from the woman.
For example:
- 12-14 oocytes retrieved
- 10-12 mature ooctyes (available for fertilization)
- 8-10 oocytes successfully fertilize with sperm
- 3-6 embryos survive and are available for transfer or storage in liquid nitrogen for future use

From the few embryos left on day five of fertilization, we try to transfer the smallest number needed to achieve a pregnancy. Approximately, one-third of the patients will have enough extra embryos to freeze for future use.
These embryos may last for decades frozen in liquid nitrogen (Mazur P, 1980). For many, deciding what to do with the embryos is a very difficult decision. In general, the following options exist:
- Thaw and transfer for personal use
- Donate to science
- — Human embryonic stem cell research
- — Other valuable studies
- Discard
- — Thaw and dispose
- — “Compassionate Transfer” into a uterus at a time when implantation cannot occur
- Donate to patients in need (i.e., embryo donation)
Many, but not all facilities, offer the “discard” option. We believe that better choices exist than destruction and no longer include it in our patient consents. The actual options available to a given patient may be more limited than the list above.
There are many reasons patients do not use the embryos for personal use (Kirkman M, 2003):
- They have completed their family
- Past pregnancy complications
- Age
- Emotional exhaustion
- Cannot afford further treatment
- Divorced
Many find deciding the next steps for their cryopreserved embryos to be exquisitely difficult. I feel that all reproductive facilities could perform far better at counseling patients and assisting them in making these decisions. Patients have complained that we haven’t done an adequate job (Nachtigall RD, et al., 2005). I suspect they are right. I believe it is the responsibility of the cryopreservation or reproductive endocrine facility to educate patients adequately and offer assistance and information when requested. EDI designed a brief brochure to address these very issues.
If one is really uncertain and the personal use of the embryos is still a possibility, then I agree that the embryos should be stored longer, but not indefinitely.  If, however, additional family building has been ruled out, then I advise the patient to take a deep breath and make the difficult decision that ultimately must be made.
If, however, additional family building has been ruled out, then I advise the patient to take a deep breath and make the difficult decision that ultimately must be made.
My patients put so much, emotionally and financially, into the creation of their embryos. Our goal is to support them through the difficult decision, no matter what they decide. I can only hope they will consider either human embryonic stem cell research or embryo donation. I personally believe embryos deserve a heightened level of respect. These two possible destinations serve a common and greater good for everyone involved. While human embryonic stem cell research holds some future promise, the immediacy of growing a family though embryo donation seems to be the best choice for those wonderful and precious gifts, a donors’ embryos.
Craig R. Sweet, M.D.
Founder, Embryo Donation International
Reproductive Endocrinologist
Medical & Laboratory Director
References:
- Kirkman M. Egg and Embryo Donation and the Meaning of Motherhood. Women & Health 2003;38(2):1-18.
- Mazur P. Limits to life at low temperatures and at reduce water contents and water activities. Orig Life 1980:10(2):137-59.
- Nachtigall RD,et al. Parents’ conceptualization of their frozen embryos complicates the disposition decision. Fertil Steril 2005;84:431-4.
Welcome to Embryo Donation International
Hello and welcome to the Embryo Donation International blog! We will be discussing all things related to embryo donation – the process, guidelines, regulations and the tough decisions that go into the final decision.
Who is Embryo Donation International (EDI)?
Embryo Donation International (EDI) is a subdivision of Specialists In Reproductive Medicine & Surgery, P.A., which has been providing embryo donation for 10 years making us one of the most experienced embryo donation facilities in the country.
Our mission is to reduce the number of cryopreserved embryos abandoned or discarded by assisting in the matching embryos to patients in need regardless of race, religion, ancestry, sexual preference or marital status. We turned this philosophy into Embryo Donation International.
I started creating our embryo donation program in 2000 and had our first delivery in 2001. I have always enjoyed the field of reproductive ethics, which helped to form many of my philosophies regarding embryo donation. In speaking out against embryo abandonment and the discarding of embryos while speaking out in favor of human embryonic stem cell research, my reproductive endocrine practice began to form the core values we now hold so dearly here at EDI.
At EDI, we believe that the embryos deserve a heightened level of respect; placing them between common cells and the patients we treat. We feel this is a type of gentle embryo advocacy. We believe that they should be used for a common good and have the opportunity to build a family.
For more information, please view the About Us section of the blog or visit our website www.EmbryoDonation.com.
What sets EDI Apart from other Embryo Donation Organizations?
EDI is non-discriminatory. We welcome healthy recipients including single women, homosexual couples, cancer survivors and people of any race or ethnicity. While we believe all healthy embryos deserve a chance at life and that healthy individual deserves a chance at parenthood, we are not a faith-based facility.
We are dedicated to making the process of embryo donation affordable. Our fees are roughly 50-60% less than many alternatives. We also accept embryos from around the world.
Additionally, we have a growing database of embryos (which is available for reviewing at no cost) and we offer them through a variety of means – approved, anonymous and open embryo donation procedures– based on the donors’ wishes and the recipients’ willingness to participate.
We look forward to offering tools for donating or receiving, or simply helping you learn more about the options available along your infertility journey, which we all hope will end with parenthood.
Craig R. Sweet, M.D.
Founder, Embryo Donation International
Reproductive Endocrinologist
Medical & Laboratory Director